Women's & Men's Health
Impact of Pre-Procedural Medications on Prostate Artery Embolization Outcomes

Piyush Goyal, n/a (he/him/his)
Medical Student
Northwestern University Feinberg School of MedicineDisclosure(s): No financial relationships to disclose
- KJ
Kimberly Jenkins, n/a
Patient Care Coordinator
Northwestern Memorial Hospital 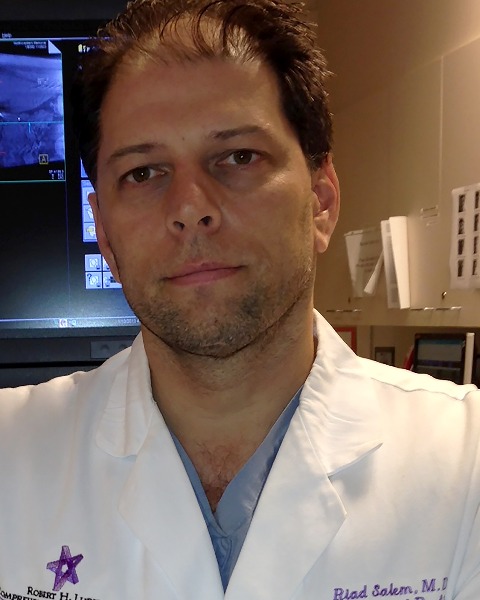
Riad Salem, MD
Chief of Vascular and Interventional Radiology in the Department of Radiology
Northwestern Memorial Hospital
Samdeep Mouli, MD
Associate Professor
Northwestern University Feinberg School of Medicine
Presenting Author(s)
Author/Co-author(s)
Medical therapy is first line management for lower urinary tract symptoms (LUTS) due to benign prostate hyperplasia (BPH) {1}. However, many patients seeking to avoid medication related adverse events pursue prostate artery embolization (PAE) to decrease utilization of BPH medications. While significant patients are able to eliminate BPH medication use, the impact of these medications on pre-procedural baseline LUTS and post-procedural outcomes is unknown. Furthermore, PAE is often performed on older patients with atherosclerosis. The purpose of this study was to report whether BPH medications or statins impact PAE outcomes.
Materials and Methods:
This was a single-center IRB-approved retrospective study. All patients who underwent PAE between June 2015 and September 2022 and had at least 1-month follow up were evaluated for pre-procedural α-blocker, 5-α-reductase inhibitor, PDE5 inhibitor and/or statin use. Multivariate regression was used to determine impact of medication use on baseline International Prostate Symptom Score (IPSS), Quality of Life (QoL) and post-procedural IPSS, QoL, Index of Erectile Function (IIEF-EF) and Male Sexual Health Questionnaire (MSHQ) outcomes.
Results:
A total of 131 patients with ≥1-month follow up were identified. Mean patient age was 68.3±8.7 years. Mean baseline and follow-up IPSS scores were 23.6±5.9 and 12.1±7.7 respectively (p < 0.01). Mean baseline and follow-up QoL scores were 4.9±0.9 and 2.6±1.5 respectively (p < 0.01). Prior to PAE, 41 patients (31.3%) were taking statins, 79 patients (60.3%) were taking alpha-blockers, 29 patients (22.1%) were taking 5-alpha-reductase inhibitors, and 28 patients (21.4%) were taking PDE5 inhibitors. Regression model outputted the impact (β coefficient) of each medication use, with age as a confounder, on PAE outcomes.
Conclusion:
Only age was significantly associated with a lower baseline QoL (β = -0.02 ± 0.01, p< 0.05) and lower ∆QoL (β = -0.05 ± 0.02, p< 0.05) improvement after PAE. Pre-procedural α-blocker use was associated with significant improvement in MSHQ ejaculatory function (β = 2.58 ± 1.10, p< 0.05). Statins, 5-α-reductase inhibitors and PDE5 inhibitors had no significant impact on measured post-procedural PAE outcomes. Interrogation of BPH medications on long-term PAE outcomes is warranted.

.png)
.png)
.jpg)
.jpg)
.png)
.png)
.png)
.jpg)
.png)