Back
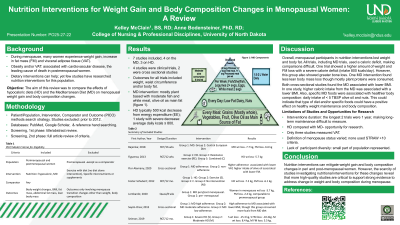
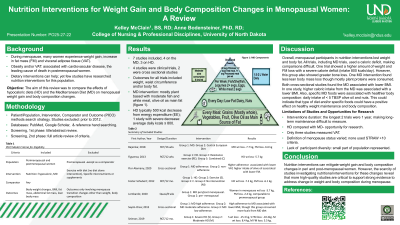
Objectives: During menopause many women experience weight gain and significant changes in body composition, including increase in visceral adipose tissue (VAT). Obesity and increased fat mass are both associated with comorbidities such as cardiovascular disease, which is the leading cause of death in postmenopausal women. Dietary interventions can address weight and body composition changes; however, few studies have researched nutrition interventions for this population. The aim of this review is to compare the effects of hypocaloric diets and the Mediterranean Diet (MD) on menopausal weight gain and body composition changes.
Methods: A literature search was conducted using Pubmed, Google Scholar, and reference hand searching. Screening included hypocaloric diets (including intermittent fasting) and MD interventions for peri and post-menopausal women. Studies excluded were studies that combined diet and exercise interventions without a separate nutrition intervention, nutrition interventions based solely on a micronutrient, studies that included premenopausal participants (unless as a comparator), and outcomes that did not include weight and/or body composition. Of the 51 screened articles, 7 matched the inclusion criteria.
Results: Four of the 7 studies were randomized controlled trials (RCTs), two were cross-sectional studies, and one was a quasi-experimental study. All experimental studies found both hypocaloric diets and the MD may decrease weight and VAT. The two cross-sectional studies showed associations between lower BMI and VAT with increased adherence to the MD. One study found that severe caloric restriction may be associated with bone density loss. The studies differed in the classification of menopausal stages.
Conclusions: These findings suggest both hypocaloric diets and the MD may reduce body weight and decrease VAT in peri and post-menopausal women. However, there are few studies addressing nutrition interventions for this population. More high quality studies are needed to examine these important menopausal changes and nutrition interventions.
Funding Sources: None
Obesity
(PO25-27-22) Nutrition Interventions for Weight Gain and Body Composition Changes in Menopausal Women: A Review
- KM
Kelley McClain, MS, RD
– Graduate Student, University of North Dakota, Lockhart, Texas, United States - AB
Anne Bodensteiner, Ph.D., RDN, LRD
– University of North Dakota
Presenting Author(s)
Co-Author(s)
Disclosure(s):
Kelley McClain, MS, RD: No relevant financial relationship(s) with ineligible companies to disclose.
Objectives: During menopause many women experience weight gain and significant changes in body composition, including increase in visceral adipose tissue (VAT). Obesity and increased fat mass are both associated with comorbidities such as cardiovascular disease, which is the leading cause of death in postmenopausal women. Dietary interventions can address weight and body composition changes; however, few studies have researched nutrition interventions for this population. The aim of this review is to compare the effects of hypocaloric diets and the Mediterranean Diet (MD) on menopausal weight gain and body composition changes.
Methods: A literature search was conducted using Pubmed, Google Scholar, and reference hand searching. Screening included hypocaloric diets (including intermittent fasting) and MD interventions for peri and post-menopausal women. Studies excluded were studies that combined diet and exercise interventions without a separate nutrition intervention, nutrition interventions based solely on a micronutrient, studies that included premenopausal participants (unless as a comparator), and outcomes that did not include weight and/or body composition. Of the 51 screened articles, 7 matched the inclusion criteria.
Results: Four of the 7 studies were randomized controlled trials (RCTs), two were cross-sectional studies, and one was a quasi-experimental study. All experimental studies found both hypocaloric diets and the MD may decrease weight and VAT. The two cross-sectional studies showed associations between lower BMI and VAT with increased adherence to the MD. One study found that severe caloric restriction may be associated with bone density loss. The studies differed in the classification of menopausal stages.
Conclusions: These findings suggest both hypocaloric diets and the MD may reduce body weight and decrease VAT in peri and post-menopausal women. However, there are few studies addressing nutrition interventions for this population. More high quality studies are needed to examine these important menopausal changes and nutrition interventions.
Funding Sources: None

.png)
