Back
Objectives: Obesity, fitness and other risk factor data for Native Hawaiians and Other Pacific Islanders (NHOPI) are frequently aggregated with Asians, who comprise the largest proportion of the Asian and Pacific Islanders (API) race/ethnic category. However, NHOPI compared with Asians are more at-risk and have higher obesity-related morbidity and mortality outcomes. Aggregated data may not provide accurate NHOPI health outcomes data. Therefore, our objective was to measure differences between fitness, obesity and other risk factors in Pacific Islanders (PIs) compared with Asian young adults.
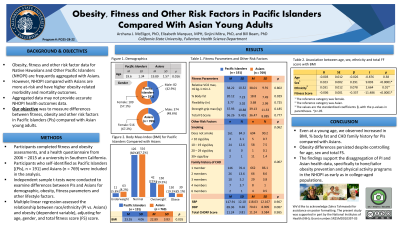
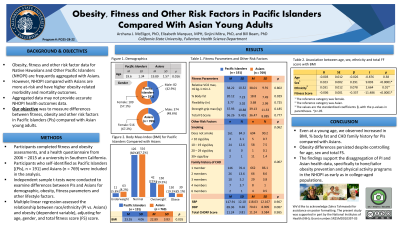
Methods: Participants completed fitness and obesity assessments, and a health questionnaire from 2006 – 2015 at a university in Southern California. Participants who self-identified as PIs (n = 191) and Asians (n = 769) were included in the analysis. Independent sample t-tests were conducted to examine differences between PIs and Asians for descriptive statistics, blood pressure, smoking, family history of coronary heart disease (CHD), as well as fitness parameters, including percent (%) body fat, relative VO2 max, strength grip, body mass index (BMI) and overall total fitness score (FS). Multiple linear regression was used to investigate the relationship between race/ethnicity (PI vs. Asians) and obesity (dependent variable), adjusting for age, gender, and total FS score.
Results: Pacific Islander young adults showed significantly higher BMI (23.55 ± 4.06 vs. 22.89 ± 3.83; p = 0.035), percent body fat (20.12 ± 7.23 vs. 18.80 ± 7.49; p = 0.029), and higher family history of CHD (p = 0.007) compared to Asians. When controlling for age, gender, and total FS score, significant (p = 0.035) differences in BMI between PIs and Asian young adults persisted. In addition, when comparing BMI by total FS score, PI young adults had significantly higher BMI compared with Asians for only moderate FS scores.
Conclusions: Even at a young age, we observed increased BMI, % body fat and CHD family history for PIs compared with Asians. Obesity differences persisted despite controlling for age, sex and total FS. The findings support the disaggregation of PI and Asian health data, specifically to hone/tailor obesity prevention and physical activity programs in the NHOPI as early as in college-aged populations.
Funding Sources: NIH
Obesity
(PO25-28-22) Obesity, Fitness and Other Risk Factors in Pacific Islanders Compared With Asian Young Adults

Archana J. McEligot, PhD
– Professor, CSUF, Fullerton, California, United States- BB
Bill Beam
– CSUF - EM
Elizabeth Marquez
– CSUF - SM
Sinjini Mitra
– CSUF
Presenting Author(s)
Co-Author(s)
Disclosure(s):
Archana J. McEligot, PhD: No relevant financial relationship(s) with ineligible companies to disclose.
Objectives: Obesity, fitness and other risk factor data for Native Hawaiians and Other Pacific Islanders (NHOPI) are frequently aggregated with Asians, who comprise the largest proportion of the Asian and Pacific Islanders (API) race/ethnic category. However, NHOPI compared with Asians are more at-risk and have higher obesity-related morbidity and mortality outcomes. Aggregated data may not provide accurate NHOPI health outcomes data. Therefore, our objective was to measure differences between fitness, obesity and other risk factors in Pacific Islanders (PIs) compared with Asian young adults.
Methods: Participants completed fitness and obesity assessments, and a health questionnaire from 2006 – 2015 at a university in Southern California. Participants who self-identified as PIs (n = 191) and Asians (n = 769) were included in the analysis. Independent sample t-tests were conducted to examine differences between PIs and Asians for descriptive statistics, blood pressure, smoking, family history of coronary heart disease (CHD), as well as fitness parameters, including percent (%) body fat, relative VO2 max, strength grip, body mass index (BMI) and overall total fitness score (FS). Multiple linear regression was used to investigate the relationship between race/ethnicity (PI vs. Asians) and obesity (dependent variable), adjusting for age, gender, and total FS score.
Results: Pacific Islander young adults showed significantly higher BMI (23.55 ± 4.06 vs. 22.89 ± 3.83; p = 0.035), percent body fat (20.12 ± 7.23 vs. 18.80 ± 7.49; p = 0.029), and higher family history of CHD (p = 0.007) compared to Asians. When controlling for age, gender, and total FS score, significant (p = 0.035) differences in BMI between PIs and Asian young adults persisted. In addition, when comparing BMI by total FS score, PI young adults had significantly higher BMI compared with Asians for only moderate FS scores.
Conclusions: Even at a young age, we observed increased BMI, % body fat and CHD family history for PIs compared with Asians. Obesity differences persisted despite controlling for age, sex and total FS. The findings support the disaggregation of PI and Asian health data, specifically to hone/tailor obesity prevention and physical activity programs in the NHOPI as early as in college-aged populations.
Funding Sources: NIH

.png)
