Back

(110) Decreased Stigma & Increased Health Equity through SUD Focused Nurse Practitioner Education
Saturday, April 2, 2022
10:00 AM – 11:30 AM ET
Location: Great Hall Foyer, Third Floor
Has Audio

Michelle Anderson, DNP, APRN, FNP-BC, FAANP
Clinical Assistant Professor
Idaho State University, Idaho
Gina Clarkson, PhD, APRN, NNP-BC
Associate Professor
Idaho State University, Idaho
Presenter(s)
Introduction: Nurse Practitioners (NPs) are large providers of primary care and are treating patients with SUD at an increasing frequency. Research shows healthcare providers lack appropriate education and training when working with SUD patients and often project negative attitudes, such as stigma (Meltzer et al., 2013; van Boekel et al., 2013). Negative attitudes and stigma are known to reduce equity in healthcare (Ashford, et al., 2019). Educational institutions are looking at ways to provide knowledge and tools needed to decrease SUD stigma and improve health equity for this population (Mitchell et al., 2020; Wakeman, et al., 2016).
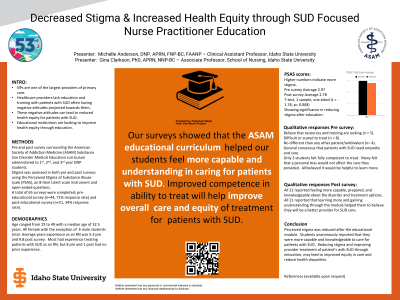
Methods: Following Institutional Review Board exemption, NP students in a Doctor of Nursing practice (DNP) program were anonymously and voluntarily surveyed about preparedness and competence in treating SUD patients and their perceived stigma. Students (n=62) were asked to complete a pre and post survey surrounding the American Society of Addiction Medicine (ASAM) Substance Use Disorder Medical Education curriculum. Stigma was assessed in both pre and post surveys using the Perceived Stigma of Substance Abuse scale (PSAS), an 8-item Likert scale instrument. A total of 65 surveys were completed; pre-educational survey (n=44, 71% response rate) and post-educational survey (n=21, 34% response rate). The students were at varying levels of experience in the program with 18 students in the 1st year, 18 students in the 2nd year, 7 students in the 3rd year, and 1 post-master’s student.
Results: Students generally felt anxious, scared, and underprepared when faced with treating a patient with SUD prior to the curriculum. Post curriculum, students reported feelings of understanding, compassion, and belief that SUD is a disease in need of treatment rather than a deficiency of the person. The students unanimously reported an improved level of competence in caring for SUD patients following the educational curriculum; 95% (n=20) reported feeling more capable and 100% (n = 21) reported feeling more able to understand, whereas pre-survey only 10% of (4 out of 43) students reported feeling competent.
Conclusions: Our surveys showed that the ASAM educational curriculum helped our students feel more capable and understanding in caring for SUD patients. We theorize that improved competence in ability to treat will help improve overall care and equity of treatment for patients with SUD. Curricula focused on reduced stigma and proper treatment is needed. Future research should continue to focus on partnerships with experts in the field of SUD, such as ASAM, to connect improvement in student self-described competence with actual improvements in care of patients with SUD.
References:
Ashford R.D., Brown A.M., McDaniel J., Curtis B. (2019). Biased labels: An experimental study of language and stigma among individuals in recovery and health professionals. Substance Use Misuse. 54(8), 1376-1384. doi: 10.1080/10826084.2019.1581221.
Meltzer, E., Suppes, A., Burns, S., Shuman, A., Orfanos, A., Sturiano, C., Charney, P., & Fins, J. (2013). Stigmatization of substance use disorders among internal medicine residents, Substance Abuse, 34(4), 356-362, DOI: 10.1080/08897077.2013.815143.
Mitchell A.M., Mahmoud K.F., Finnell D., Savage C.L., Weber M., & Bacidore V. (2020). The essentials competencies: A framework for substance use-related curricula. Nurse Educator. 45(4), 225-228. doi: 10.1097/NNE.0000000000000753. PMID: 31634219.
Van Boekel, L.C., Brouwers, E.P.M., van Weedhel, J., & Garretsena, H.F.L. (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence, 131, 23-35. https://dx.doi.org/10.1016/j.drugalcdep.2013.02.018
Wakeman, S.E., Pham-Kanter, G., & Donelan, K.(2016) Attitudes, practices, and preparedness to care for patients with substance use disorder: Results from a survey of general internists, Substance Abuse, 37(4), 635-641, DOI: 10.1080/08897077.2016.1187240.
Methods: Following Institutional Review Board exemption, NP students in a Doctor of Nursing practice (DNP) program were anonymously and voluntarily surveyed about preparedness and competence in treating SUD patients and their perceived stigma. Students (n=62) were asked to complete a pre and post survey surrounding the American Society of Addiction Medicine (ASAM) Substance Use Disorder Medical Education curriculum. Stigma was assessed in both pre and post surveys using the Perceived Stigma of Substance Abuse scale (PSAS), an 8-item Likert scale instrument. A total of 65 surveys were completed; pre-educational survey (n=44, 71% response rate) and post-educational survey (n=21, 34% response rate). The students were at varying levels of experience in the program with 18 students in the 1st year, 18 students in the 2nd year, 7 students in the 3rd year, and 1 post-master’s student.
Results: Students generally felt anxious, scared, and underprepared when faced with treating a patient with SUD prior to the curriculum. Post curriculum, students reported feelings of understanding, compassion, and belief that SUD is a disease in need of treatment rather than a deficiency of the person. The students unanimously reported an improved level of competence in caring for SUD patients following the educational curriculum; 95% (n=20) reported feeling more capable and 100% (n = 21) reported feeling more able to understand, whereas pre-survey only 10% of (4 out of 43) students reported feeling competent.
Conclusions: Our surveys showed that the ASAM educational curriculum helped our students feel more capable and understanding in caring for SUD patients. We theorize that improved competence in ability to treat will help improve overall care and equity of treatment for patients with SUD. Curricula focused on reduced stigma and proper treatment is needed. Future research should continue to focus on partnerships with experts in the field of SUD, such as ASAM, to connect improvement in student self-described competence with actual improvements in care of patients with SUD.
References:
Ashford R.D., Brown A.M., McDaniel J., Curtis B. (2019). Biased labels: An experimental study of language and stigma among individuals in recovery and health professionals. Substance Use Misuse. 54(8), 1376-1384. doi: 10.1080/10826084.2019.1581221.
Meltzer, E., Suppes, A., Burns, S., Shuman, A., Orfanos, A., Sturiano, C., Charney, P., & Fins, J. (2013). Stigmatization of substance use disorders among internal medicine residents, Substance Abuse, 34(4), 356-362, DOI: 10.1080/08897077.2013.815143.
Mitchell A.M., Mahmoud K.F., Finnell D., Savage C.L., Weber M., & Bacidore V. (2020). The essentials competencies: A framework for substance use-related curricula. Nurse Educator. 45(4), 225-228. doi: 10.1097/NNE.0000000000000753. PMID: 31634219.
Van Boekel, L.C., Brouwers, E.P.M., van Weedhel, J., & Garretsena, H.F.L. (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence, 131, 23-35. https://dx.doi.org/10.1016/j.drugalcdep.2013.02.018
Wakeman, S.E., Pham-Kanter, G., & Donelan, K.(2016) Attitudes, practices, and preparedness to care for patients with substance use disorder: Results from a survey of general internists, Substance Abuse, 37(4), 635-641, DOI: 10.1080/08897077.2016.1187240.
