Back

(81) Low-Barrier Group Medical Visits for Substance Use Disorder
Saturday, April 2, 2022
10:00 AM – 11:30 AM ET
Location: Great Hall Foyer, Third Floor
Has Audio

Paula J. Cook, MD, DFASAM
Faculty physician
Utah Healthcare Institute, Utah- CO
Corey Ordnorff, BSc
Community Health Worker
Martindale Clinic, Utah
Presenter(s)
Non-presenting author(s)
Introduction/
Background:
Access to addiction treatment, especially rapid access to buprenorphine/naloxone, has proven efficacy in assisting those with opioid use disorder (OUD)1. Access to harm reduction services is additionally important for people who use drugs (PWUDs), as they have high rates of skin and blood-borne infections, overdose, and suicide2,3. Group medical visits (GMVs) have been effectively used in addiction treatment settings, proving that the group delivery of medications for opioid use disorder (MOUD) is feasible and has added inherent benefits from the coupling of group counseling and shared peer experience4. The research hypothesis was that provision of GMVs with wrap-around services would engage and retain patients who needed access to MOUD as well as harm reduction services in a non-conventional model, with outcomes measured by tracking attendance, patient retention, and pursuit of integrated services throughout the project period.
Methods:
Low-barrier GMVs were made available to patients not thriving within the traditional medical model (e.g frequently missed or late appointments, inconsistent use of MOUD, or ongoing substance use). The groups were attended by a staff team that included a group therapist facilitator, a peer support specialist, a harm reduction navigator, and a provider/medical assistant team. GMVs were held 2-3 times weekly during the project period from February-August 2021. The GMV process involved an hour-long group, facilitated by the therapist and peer-support specialist. Patients were called out individually to meet with the provider to address MOUD needs. This visit focused on patient-centered treatment goals using motivational enhancement. Harm reduction services and education, including syringe exchange services, safer injection kits, safer sex kits, STI testing, naloxone, fentanyl test strips, and gun locks were offered to every participant. Ear acupuncture, assistance with Medicaid applications and referrals to community resources, as well as coffee and snacks were also provided. Allowing walk-ins to the GMVs, maintaining a liberal late check-in cut-off, and accepting patients regardless of sobriety status ensured the groups remained available to patients who could benefit most from low-barrier access to SUD treatment.
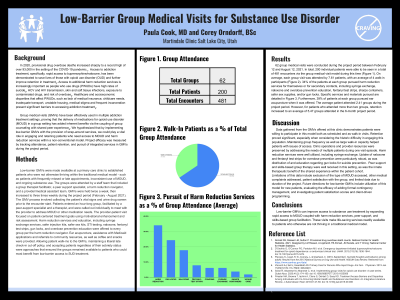
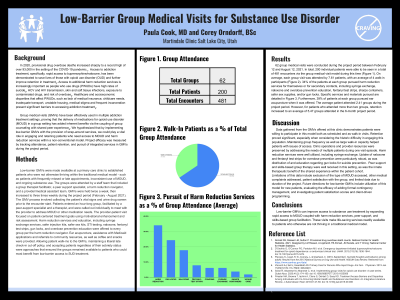
Results:
62 group medical visits were conducted between February and August 2021. 200 individual patients were seen in a total of 481 encounters. On average, each group visit was attended by 7.61 patients, with an average of 4 walk-in participants. 34% of the patients at each group pursued harm reduction services. 39% of patients at each group pursued ear acupuncture. The average patient attended 2.41 groups during the project period. However, considering patients who attended more than two groups, retention increased to an average of 5.47 groups attended.
Discussion:
GMV data demonstrates patients were willing to participate in this model, both as scheduled and walk-in visits. Retention proved significant, especially when considering the historic difficulty in engaging this population. Maintaining group frequency as well as large walk-in capacity helped patients with issues of access. Harm reduction services were well utilized, and peer support and skills-based group therapy were well-received in this setting.
Conclusion:
Low-barrier GMVs can improve access to addiction treatment by expanding rapid access to MOUD coupled with harm reduction services, peer support, and skills-based group facilitation. These visits make life-saving services readily available to patients who otherwise are not thriving in a traditional medical model.
References
1. D'Onofrio G, O'Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636-1644. doi:10.1001/jama.2015.3474
2. Piscopo, K., Lipari, R. N., Cooney, J., & Glasheen, C. (2016, September). Suicidal thoughts and behavior among adults: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review. Retrieved from https://link.zixcentral.com/u/81b03d04/2lR70Xhy7BGtp1nGhnsoMg?u=https%3A%2F%2Fwww.samhsa.gov%2Fdata%2F
3. Visconti AJ, Sell J, Greenblatt AD. Primary Care for Persons Who Inject Drugs. Am Fam Physician. 2019 Jan 15;99(2):109-116. PMID: 30633481.
4. Sokol R, Albanese M, Albanese C, et al. Implementing group visits for opioid use disorder: A case series. Subst Abus. 2020;41(2):174-180. doi:10.1080/08897077.2019.1635958
5. Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment Access Barriers and Disparities Among Individuals with Co-Occurring Mental Health and Substance Use Disorders: An Integrative Literature Review. J Subst Abuse Treat. 2016;61:47-59. doi:10.1016/j.jsat.2015.09.006
Diversity, Equity, and Inclusion:
This program specifically targets patients who are not successfully accessing care due to healthcare and socioeconomic disparities including poverty, lack of medical insurance, lack of childcare, inadequate transport, unstable housing, history of experiencing medical stigma and trauma, and frequent incarceration. Diversity is accounted for and welcomed in a "come as you are" manner, with a trauma informed, gender and ethnicity sensitive staff focused on harm reduction and strong peer support and skills based facilitation.
Background:
Access to addiction treatment, especially rapid access to buprenorphine/naloxone, has proven efficacy in assisting those with opioid use disorder (OUD)1. Access to harm reduction services is additionally important for people who use drugs (PWUDs), as they have high rates of skin and blood-borne infections, overdose, and suicide2,3. Group medical visits (GMVs) have been effectively used in addiction treatment settings, proving that the group delivery of medications for opioid use disorder (MOUD) is feasible and has added inherent benefits from the coupling of group counseling and shared peer experience4. The research hypothesis was that provision of GMVs with wrap-around services would engage and retain patients who needed access to MOUD as well as harm reduction services in a non-conventional model, with outcomes measured by tracking attendance, patient retention, and pursuit of integrated services throughout the project period.
Methods:
Low-barrier GMVs were made available to patients not thriving within the traditional medical model (e.g frequently missed or late appointments, inconsistent use of MOUD, or ongoing substance use). The groups were attended by a staff team that included a group therapist facilitator, a peer support specialist, a harm reduction navigator, and a provider/medical assistant team. GMVs were held 2-3 times weekly during the project period from February-August 2021. The GMV process involved an hour-long group, facilitated by the therapist and peer-support specialist. Patients were called out individually to meet with the provider to address MOUD needs. This visit focused on patient-centered treatment goals using motivational enhancement. Harm reduction services and education, including syringe exchange services, safer injection kits, safer sex kits, STI testing, naloxone, fentanyl test strips, and gun locks were offered to every participant. Ear acupuncture, assistance with Medicaid applications and referrals to community resources, as well as coffee and snacks were also provided. Allowing walk-ins to the GMVs, maintaining a liberal late check-in cut-off, and accepting patients regardless of sobriety status ensured the groups remained available to patients who could benefit most from low-barrier access to SUD treatment.
Results:
62 group medical visits were conducted between February and August 2021. 200 individual patients were seen in a total of 481 encounters. On average, each group visit was attended by 7.61 patients, with an average of 4 walk-in participants. 34% of the patients at each group pursued harm reduction services. 39% of patients at each group pursued ear acupuncture. The average patient attended 2.41 groups during the project period. However, considering patients who attended more than two groups, retention increased to an average of 5.47 groups attended.
Discussion:
GMV data demonstrates patients were willing to participate in this model, both as scheduled and walk-in visits. Retention proved significant, especially when considering the historic difficulty in engaging this population. Maintaining group frequency as well as large walk-in capacity helped patients with issues of access. Harm reduction services were well utilized, and peer support and skills-based group therapy were well-received in this setting.
Conclusion:
Low-barrier GMVs can improve access to addiction treatment by expanding rapid access to MOUD coupled with harm reduction services, peer support, and skills-based group facilitation. These visits make life-saving services readily available to patients who otherwise are not thriving in a traditional medical model.
References
1. D'Onofrio G, O'Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636-1644. doi:10.1001/jama.2015.3474
2. Piscopo, K., Lipari, R. N., Cooney, J., & Glasheen, C. (2016, September). Suicidal thoughts and behavior among adults: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review. Retrieved from https://link.zixcentral.com/u/81b03d04/2lR70Xhy7BGtp1nGhnsoMg?u=https%3A%2F%2Fwww.samhsa.gov%2Fdata%2F
3. Visconti AJ, Sell J, Greenblatt AD. Primary Care for Persons Who Inject Drugs. Am Fam Physician. 2019 Jan 15;99(2):109-116. PMID: 30633481.
4. Sokol R, Albanese M, Albanese C, et al. Implementing group visits for opioid use disorder: A case series. Subst Abus. 2020;41(2):174-180. doi:10.1080/08897077.2019.1635958
5. Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment Access Barriers and Disparities Among Individuals with Co-Occurring Mental Health and Substance Use Disorders: An Integrative Literature Review. J Subst Abuse Treat. 2016;61:47-59. doi:10.1016/j.jsat.2015.09.006
Diversity, Equity, and Inclusion:
This program specifically targets patients who are not successfully accessing care due to healthcare and socioeconomic disparities including poverty, lack of medical insurance, lack of childcare, inadequate transport, unstable housing, history of experiencing medical stigma and trauma, and frequent incarceration. Diversity is accounted for and welcomed in a "come as you are" manner, with a trauma informed, gender and ethnicity sensitive staff focused on harm reduction and strong peer support and skills based facilitation.
