Back

(20) U.S. County Jail Care of Incarcerated Pregnant Persons with Opioid Use Disorder
Friday, April 1, 2022
11:30 AM – 1:00 PM ET
Location: Great Hall Foyer, Third Floor
Has Audio

Kelley Benck
Medical Student
University of Miami Miller School of Medicine, Florida- AJ
Alexis K. Jones, BS
Medical Student
University of Miami, Florida - KN
Kathryn M. Nowotny, PhD
Associate Professor
University of Miami, Florida
Presenter(s)
Non-presenting author(s)
Introduction:
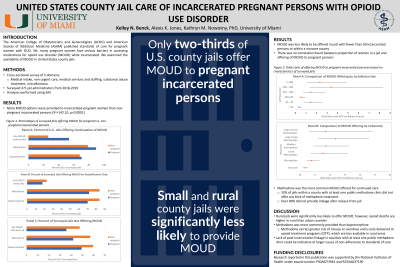
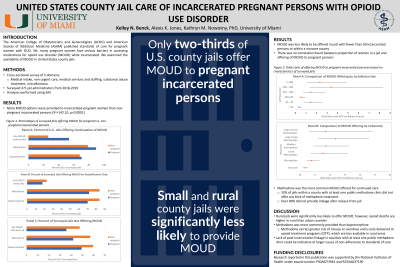
The American College of Obstetricians and Gynecologists (ACOG) and American Society of Addiction Medicine (ASAM) published standards of care for pregnant persons with opioid use disorder (OUD). Yet, many pregnant persons face serious barriers in accessing medications for opioid use disorder (MOUD) while incarcerated. We examined the availability of MOUD in U.S. jails.
Methods:
Data are from a cross-sectional survey of jail administrators (2018-2019; n=371), including five domains: medical intake, non-urgent care, medical services and staffing, substance abuse treatment, and miscellaneous. Analyses were performed using SAS.
Results:
More MOUD options were provided to incarcerated pregnant persons than non-pregnant incarcerated persons (X2=142.10, p < 0.0001). Jurisdiction size and urbanicity significantly impacted whether MOUD was offered (X2=30.12, p < 0.0001; X2=26.46, p < 0.0001), and offering this care was less likely in jails with fewer than 50 incarcerated persons (OR 0.35, 95% CI: 0.21-0.61) or within a noncore county (OR 0.33, 95% CI: 0.20–0.54). Methadone was the most common MOUD offered for continued care for both pregnant and non-pregnant incarcerated persons. Of the 144 jails within a county with at least one public methadone clinic, 33% did not offer any kind of methadone treatment, and over 80% did not provide linkage after release from jail.
Conclusion:
Overall, only about two-thirds of surveyed jails offered any sort of MOUD. Rural jails were significantly less likely to offer OUD standards of care, which is especially concerning because the number of opioid deaths in rural counties continues to surpass those in urban counties. Interestingly, methadone was more commonly provided than buprenorphine even though it carries a greater risk of misuse or overdose and can only be delivered at strictly regulated opioid treatment programs (OTP), which tend to be less available in rural areas. In addition, the significant lack of post-incarceration linkage in counties with at least one public methadone clinic could be indicative of larger issues surrounding adherence to published MOUD best practices. Jails can be an important turning point in the care of a pregnant person with OUD as these institutions continue to see high rates of substance misuse. Therefore, understanding how jail characteristics impact adherence to published standards of care may help better direct efforts to improve MOUD delivery.
References:
Committee Opinion No. 711: Opioid Use and Opioid Use Disorder in Pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52-59.
Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic Distribution of Providers With a DEA Waiver to Prescribe Buprenorphine for the Treatment of Opioid Use Disorder: A 5-Year Update. J Rural Health. 2019;35(1):108-112.
Fazel S, Yoon IA, Hayes AJ. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction. 2017;112(10):1725-1739.
The American College of Obstetricians and Gynecologists (ACOG) and American Society of Addiction Medicine (ASAM) published standards of care for pregnant persons with opioid use disorder (OUD). Yet, many pregnant persons face serious barriers in accessing medications for opioid use disorder (MOUD) while incarcerated. We examined the availability of MOUD in U.S. jails.
Methods:
Data are from a cross-sectional survey of jail administrators (2018-2019; n=371), including five domains: medical intake, non-urgent care, medical services and staffing, substance abuse treatment, and miscellaneous. Analyses were performed using SAS.
Results:
More MOUD options were provided to incarcerated pregnant persons than non-pregnant incarcerated persons (X2=142.10, p < 0.0001). Jurisdiction size and urbanicity significantly impacted whether MOUD was offered (X2=30.12, p < 0.0001; X2=26.46, p < 0.0001), and offering this care was less likely in jails with fewer than 50 incarcerated persons (OR 0.35, 95% CI: 0.21-0.61) or within a noncore county (OR 0.33, 95% CI: 0.20–0.54). Methadone was the most common MOUD offered for continued care for both pregnant and non-pregnant incarcerated persons. Of the 144 jails within a county with at least one public methadone clinic, 33% did not offer any kind of methadone treatment, and over 80% did not provide linkage after release from jail.
Conclusion:
Overall, only about two-thirds of surveyed jails offered any sort of MOUD. Rural jails were significantly less likely to offer OUD standards of care, which is especially concerning because the number of opioid deaths in rural counties continues to surpass those in urban counties. Interestingly, methadone was more commonly provided than buprenorphine even though it carries a greater risk of misuse or overdose and can only be delivered at strictly regulated opioid treatment programs (OTP), which tend to be less available in rural areas. In addition, the significant lack of post-incarceration linkage in counties with at least one public methadone clinic could be indicative of larger issues surrounding adherence to published MOUD best practices. Jails can be an important turning point in the care of a pregnant person with OUD as these institutions continue to see high rates of substance misuse. Therefore, understanding how jail characteristics impact adherence to published standards of care may help better direct efforts to improve MOUD delivery.
References:
Committee Opinion No. 711: Opioid Use and Opioid Use Disorder in Pregnancy. Obstet Gynecol. 2017;130(2):e81-e94.
Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52-59.
Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic Distribution of Providers With a DEA Waiver to Prescribe Buprenorphine for the Treatment of Opioid Use Disorder: A 5-Year Update. J Rural Health. 2019;35(1):108-112.
Fazel S, Yoon IA, Hayes AJ. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction. 2017;112(10):1725-1739.
