Back
Systems-Based Practice and Administrative Psychiatry
Poster Session
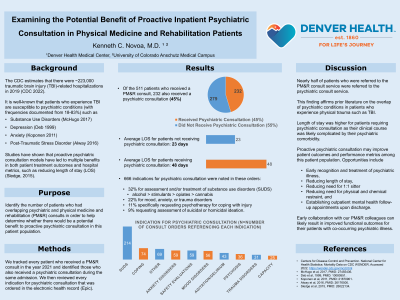
(174) Examining the Potential Benefit of Proactive Inpatient Psychiatric Consultation in Physical Medicine and Rehabilitation Patients
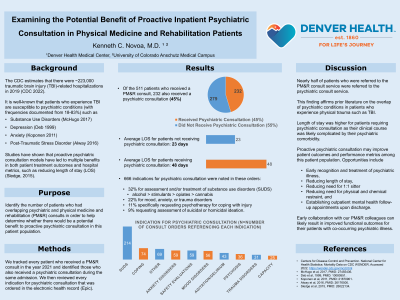
Abstract: Background
Studies have shown that proactive psychiatric consultation models have led to multiple benefits in both patient treatment outcomes and hospital metrics, such as reducing length of stay (Sledge, 2015). It is well-known that patients who experience traumatic brain injury are susceptible to psychiatric conditions such as substance use disorders (McHugo, 2017) and depression (Deb 1999). We examined data to identify the number of patients who had overlapping psychiatric and physical medicine and rehabilitation (PM&R) consults in order to determine whether there would be a potential benefit in proactive psychiatric consultation in the PM&R patient population.
Methods
Using data from our electronic medical record system, we tracked every patient who received a PM&R consult in the year 2021 and isolated those who also received a psychiatric consultation during the same admission. We then reviewed every indication for psychiatric consultation that was entered.
Results
Of the 511 patients who received a PM&R consult, 232 of them also received a psychiatric consultation (45.4%). In total, 666 reasons for psychiatric consultation were found. Of these, 32% were for assessment and/or treatment of substance use disorders (majority for alcohol use disorder), 22% for mood, anxiety, or trauma disorders, 11% specifically requesting psychotherapy, and 9% specifically asking for assessment of suicidal or homicidal ideation.
Discussion
Nearly one in two patients who were asked to see the PM&R consult service were also asked to see the psychiatric consult service. This lends credence to prior published data on the overlap of psychiatric conditions in patients who experience physical trauma. This presents us with an opportunity to provide proactive psychiatric consultation in an effort to improve patient outcomes and hospital metrics, such as early recognition and treatment of psychiatric illness, reducing length of stay, and establishing outpatient mental follow-up appointments upon discharge. This year, we would like to compare length of stay outcomes during a six-month period in this patient population between those who do and do not receive proactive psychiatric consultation.
Conclusion
The overlap in patients who require PM&R and psychiatric consultation during inpatient hospitalization is significant. We believe we could have a significant impact on improving patient treatment outcomes and hospital metrics by proactively consulting on this vulnerable patient population.
References
Sledge W, H, Gueorguieva R, Desan P, Bozzo J, E, Dorset J, Lee H, B: Multidisciplinary Proactive Psychiatric Consultation Service: Impact on Length of Stay for Medical Inpatients. Psychother Psychosom 2015;84:208-216.
McHugo GJ, Krassenbaum S, Donley S, et al: The prevalence of traumatic brain injury among people with co-occurring mental health and substance use disorders. J Head Trauma Rehabil 32(3):E65–E74, 2017
Deb S, Lyons I, Koutzoukis C, Ali I, McCarthy G. Rate of psychiatric illness 1 year after traumatic brain injury. Am J Psychiatry 1999;156:374‐8.
Studies have shown that proactive psychiatric consultation models have led to multiple benefits in both patient treatment outcomes and hospital metrics, such as reducing length of stay (Sledge, 2015). It is well-known that patients who experience traumatic brain injury are susceptible to psychiatric conditions such as substance use disorders (McHugo, 2017) and depression (Deb 1999). We examined data to identify the number of patients who had overlapping psychiatric and physical medicine and rehabilitation (PM&R) consults in order to determine whether there would be a potential benefit in proactive psychiatric consultation in the PM&R patient population.
Methods
Using data from our electronic medical record system, we tracked every patient who received a PM&R consult in the year 2021 and isolated those who also received a psychiatric consultation during the same admission. We then reviewed every indication for psychiatric consultation that was entered.
Results
Of the 511 patients who received a PM&R consult, 232 of them also received a psychiatric consultation (45.4%). In total, 666 reasons for psychiatric consultation were found. Of these, 32% were for assessment and/or treatment of substance use disorders (majority for alcohol use disorder), 22% for mood, anxiety, or trauma disorders, 11% specifically requesting psychotherapy, and 9% specifically asking for assessment of suicidal or homicidal ideation.
Discussion
Nearly one in two patients who were asked to see the PM&R consult service were also asked to see the psychiatric consult service. This lends credence to prior published data on the overlap of psychiatric conditions in patients who experience physical trauma. This presents us with an opportunity to provide proactive psychiatric consultation in an effort to improve patient outcomes and hospital metrics, such as early recognition and treatment of psychiatric illness, reducing length of stay, and establishing outpatient mental follow-up appointments upon discharge. This year, we would like to compare length of stay outcomes during a six-month period in this patient population between those who do and do not receive proactive psychiatric consultation.
Conclusion
The overlap in patients who require PM&R and psychiatric consultation during inpatient hospitalization is significant. We believe we could have a significant impact on improving patient treatment outcomes and hospital metrics by proactively consulting on this vulnerable patient population.
References
Sledge W, H, Gueorguieva R, Desan P, Bozzo J, E, Dorset J, Lee H, B: Multidisciplinary Proactive Psychiatric Consultation Service: Impact on Length of Stay for Medical Inpatients. Psychother Psychosom 2015;84:208-216.
McHugo GJ, Krassenbaum S, Donley S, et al: The prevalence of traumatic brain injury among people with co-occurring mental health and substance use disorders. J Head Trauma Rehabil 32(3):E65–E74, 2017
Deb S, Lyons I, Koutzoukis C, Ali I, McCarthy G. Rate of psychiatric illness 1 year after traumatic brain injury. Am J Psychiatry 1999;156:374‐8.
.jpg)
Kenneth Novoa, MD
Medical Director - Consultation-Liaison Psychiatry service
Denver Health Medical Center
Denver, CO, United States