Back

Aging and Dementia: Other
Traditional Poster Presentation
(115) Identifying factors related to high healthcare utilization in a group of persons with dementia and their caregivers
Has Audio
- CP
Carolina Pereira Osorio, MSc. in Psychology
Associate Clinical Research Coordinator
Ochsner Health
New Orleans, Louisiana, United States
Primary Author(s)
Objective: Identify factors related to high healthcare utilization in dementia patients to determine a high-risk profile and tailor the Care Ecosystem Program to subgroup needs.
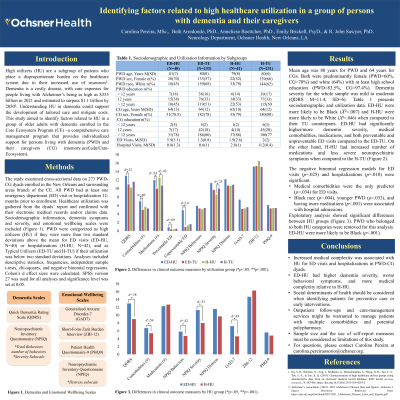
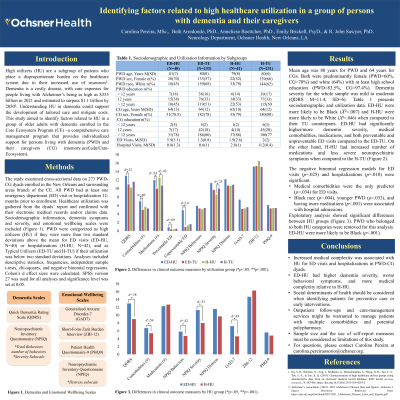
Methods: Cross-sectional data on persons with dementia (PWD) and caregivers (CG) enrolled in a branch of the Care Ecosystem Program (memory.ucsf.edu/Care-Ecosystem) were used. PWD had one emergency department (ED) visit or hospitalization prior 12-months. Data for 273 dyads included sociodemographics, healthcare utilization, dementia severity (Quick Dementia Rating Scale), and emotional wellbeing (i.e., Short-Form Zarit Burden Interview, Patient Health Questionnaire-9, Generalized Anxiety Disorder-7). High utilizers (HU) were more than two standard deviations above the mean for ED visits (N=40) or hospitalizations (N=42). Analyses included descriptive, frequencies, independent sample t-tests, and negative binomial regressions.
Results: Mean age was 80 years for PWD and 64 years for CGs. Both were predominantly female (PWD=60%, CG=78%) and white (64%) with high school education or higher (PWD=83.5%, CG=97.4%). Dementia severity was mild to moderate (QDRS M=11.4; SD=6). ED-HU had higher/more dementia severity (p=.03, d=6.2), medical comorbidities (p <.001, d=2.4), medications (p=.047, d=4.5), and preventable (p=.013, d=.7) and unpreventable (p <.001, d=1.5) visits. Hospitalization HU presented increased neuropsychiatric severity (p=.048, d=6.5) and medications (p=.012, d=4.4). Negative binomial regression model for ED visits (p=.025) showed increased comorbidities as the only predictor (p=.034), while the model for hospitalizations (p=.010) was associated with Black race (p=.004), younger PWD (p=.033), and more medications (p <.001).
Conclusions: Increased medical complexity was associated with HU for ED visits and hospitalizations in PWD-CG dyads. Additional research and possible need for variation in care management services are warranted.
Methods: Cross-sectional data on persons with dementia (PWD) and caregivers (CG) enrolled in a branch of the Care Ecosystem Program (memory.ucsf.edu/Care-Ecosystem) were used. PWD had one emergency department (ED) visit or hospitalization prior 12-months. Data for 273 dyads included sociodemographics, healthcare utilization, dementia severity (Quick Dementia Rating Scale), and emotional wellbeing (i.e., Short-Form Zarit Burden Interview, Patient Health Questionnaire-9, Generalized Anxiety Disorder-7). High utilizers (HU) were more than two standard deviations above the mean for ED visits (N=40) or hospitalizations (N=42). Analyses included descriptive, frequencies, independent sample t-tests, and negative binomial regressions.
Results: Mean age was 80 years for PWD and 64 years for CGs. Both were predominantly female (PWD=60%, CG=78%) and white (64%) with high school education or higher (PWD=83.5%, CG=97.4%). Dementia severity was mild to moderate (QDRS M=11.4; SD=6). ED-HU had higher/more dementia severity (p=.03, d=6.2), medical comorbidities (p <.001, d=2.4), medications (p=.047, d=4.5), and preventable (p=.013, d=.7) and unpreventable (p <.001, d=1.5) visits. Hospitalization HU presented increased neuropsychiatric severity (p=.048, d=6.5) and medications (p=.012, d=4.4). Negative binomial regression model for ED visits (p=.025) showed increased comorbidities as the only predictor (p=.034), while the model for hospitalizations (p=.010) was associated with Black race (p=.004), younger PWD (p=.033), and more medications (p <.001).
Conclusions: Increased medical complexity was associated with HU for ED visits and hospitalizations in PWD-CG dyads. Additional research and possible need for variation in care management services are warranted.
