Back
Transplant Psychiatry
Poster Session
(191) Cache Valley Virus Encephalitis presenting as Akinetic Mutism after Renal Transplant
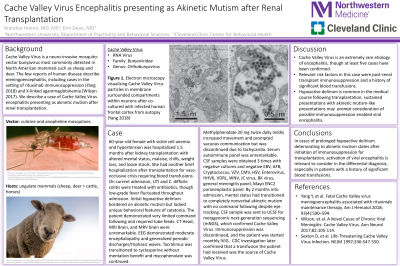
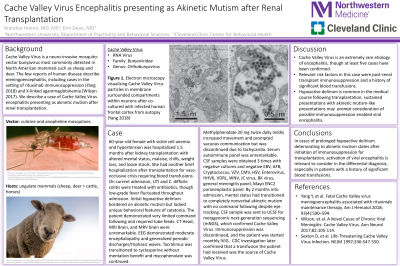
Abstract: Background
Cache Valley Virus is a neuro-invasive mosquito-vector bunyavirus most commonly detected in North American mammals such as sheep and deer. The few reports of human disease describe meningoencephalitis, including cases in the setting of rituximab immunosuppression (Yang 2018) and X-linked agammaglobinemia (Wilson 2017). We describe a case of Cache Valley Virus encephalitis presenting as akinetic mutism after renal transplantation.
Case
A 60-year-old female with sickle cell anemia and hypertension was hospitalized 1.5 months after kidney transplantation with altered mental status, malaise, chills, weight loss, and loose stools. She had brief hospitalization after transplantation for vaso-occlusive crisis requiring blood transfusions. On current admission, UTI and C. difficile colitis were treated with antibiotics, though low-grade fever fluctuated throughout admission. Initial hypoactive delirium bordered on akinetic mutism but lacked the unique behavioral features of catatonia. The patient demonstrated very limited command following and required tube feeds. CT Head, MRI Brain, and MRV brain were unremarkable. EEG demonstrated moderate encephalopathy and generalized periodic discharges/triphasic waves. Tacrolimus was transitioned to cyclosporine without mentation benefit and mycophenolate was continued, with later prednisone addition. Methylphenidate 20 mg twice daily mildly increased movement and prompted vacuous communication but was eventually discontinued due to tachycardia. Serum autoimmune panel was unremarkable. CSF samples were obtained on 3 occasions, with negative cultures, EBV, AFB, Cryptococcus, VZV, CMV, HSV, Enterovirus, HHV6, VDRL, WNV, JC virus, BK virus, viral meningitis panel, Mayo ENC2 paraneoplastic panel. Within 2 months, mental status had transitioned to complete nonverbal akinetic mutism with no command following despite eye tracking. CSF metagenomic next-generation sequencing (mNGS) confirmed presence of Cache Valley Virus. Immunosuppression was discontinued, and monthly IVIG was started. CDC investigation later confirmed that Cache Valley Virus was present in a transfusion the patient had received.
Discussion
Cache Valley Virus is an extremely rare etiology of encephalitis, though at least five cases have been confirmed. In case we describe, the relevant risk factors were post-renal transplant immunosuppression and a history of significant blood transfusions. Although hypoactive delirium is common in the medical course following transplantation, sustained neurovegitation with akinetic mutism-like presentations should prompt consideration of possible immunosuppression enabled viral encephalitis.
Conclusions
In cases of prolonged hypoactive delirium deteriorating to akinetic mutism states after initiation of immunosuppression for transplantation, activation of viral encephalitis is relevant to consider in the differential diagnosis, especially in patients with a history of significant blood transfusions.
References
Yang Y, et al. Fatal Cache Valley virus meningoencephalitis associated with rituximab maintenance therapy. Am J Hematol 2018; 93(4):590–594.
Wilson, et al. A Novel Cause of Chronic Viral Meningitis: Cache Valley Virus.Ann Neurol 2017;82:105-114.
Sexton D, et al. Life-Threatening Cache Valley Virus Infection. NEJM 1997;336:547-550.
Cache Valley Virus is a neuro-invasive mosquito-vector bunyavirus most commonly detected in North American mammals such as sheep and deer. The few reports of human disease describe meningoencephalitis, including cases in the setting of rituximab immunosuppression (Yang 2018) and X-linked agammaglobinemia (Wilson 2017). We describe a case of Cache Valley Virus encephalitis presenting as akinetic mutism after renal transplantation.
Case
A 60-year-old female with sickle cell anemia and hypertension was hospitalized 1.5 months after kidney transplantation with altered mental status, malaise, chills, weight loss, and loose stools. She had brief hospitalization after transplantation for vaso-occlusive crisis requiring blood transfusions. On current admission, UTI and C. difficile colitis were treated with antibiotics, though low-grade fever fluctuated throughout admission. Initial hypoactive delirium bordered on akinetic mutism but lacked the unique behavioral features of catatonia. The patient demonstrated very limited command following and required tube feeds. CT Head, MRI Brain, and MRV brain were unremarkable. EEG demonstrated moderate encephalopathy and generalized periodic discharges/triphasic waves. Tacrolimus was transitioned to cyclosporine without mentation benefit and mycophenolate was continued, with later prednisone addition. Methylphenidate 20 mg twice daily mildly increased movement and prompted vacuous communication but was eventually discontinued due to tachycardia. Serum autoimmune panel was unremarkable. CSF samples were obtained on 3 occasions, with negative cultures, EBV, AFB, Cryptococcus, VZV, CMV, HSV, Enterovirus, HHV6, VDRL, WNV, JC virus, BK virus, viral meningitis panel, Mayo ENC2 paraneoplastic panel. Within 2 months, mental status had transitioned to complete nonverbal akinetic mutism with no command following despite eye tracking. CSF metagenomic next-generation sequencing (mNGS) confirmed presence of Cache Valley Virus. Immunosuppression was discontinued, and monthly IVIG was started. CDC investigation later confirmed that Cache Valley Virus was present in a transfusion the patient had received.
Discussion
Cache Valley Virus is an extremely rare etiology of encephalitis, though at least five cases have been confirmed. In case we describe, the relevant risk factors were post-renal transplant immunosuppression and a history of significant blood transfusions. Although hypoactive delirium is common in the medical course following transplantation, sustained neurovegitation with akinetic mutism-like presentations should prompt consideration of possible immunosuppression enabled viral encephalitis.
Conclusions
In cases of prolonged hypoactive delirium deteriorating to akinetic mutism states after initiation of immunosuppression for transplantation, activation of viral encephalitis is relevant to consider in the differential diagnosis, especially in patients with a history of significant blood transfusions.
References
Yang Y, et al. Fatal Cache Valley virus meningoencephalitis associated with rituximab maintenance therapy. Am J Hematol 2018; 93(4):590–594.
Wilson, et al. A Novel Cause of Chronic Viral Meningitis: Cache Valley Virus.Ann Neurol 2017;82:105-114.
Sexton D, et al. Life-Threatening Cache Valley Virus Infection. NEJM 1997;336:547-550.
Brandon Hamm, MD, MS (he/him/his)
Assistant Professor, CL Psychiatrist
Northwestern University
Chicago, Illinois, United States.jpg)
Erin Dean, MD
Staff Psychiatrist
Cleveland Clinic
Cleveland, Ohio, United States