Back
Poster, Podium & Video Sessions
Moderated Poster
MP13: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making I
MP13-11: EHR-based Clinical Decision Support for Urologic Surgery: User Perspectives and Needs
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 228
Hung-Jui Tan*, Chapel Hill, NC, Brooke Spratte, Durham, NC, Allison Deal, Antonia Bennett, Susan Blalock, Chapel Hill, NC, Arlene Chung, Durham, NC, David Gotz, Matthew Nielsen, Dan Reuland, Chapel Hill, NC, Alex Sox-Harris, Stanford, CA, Ethan Basch, Chapel Hill, NC
- HT
Hung-Jui Tan, MD
University Of North Carolina at Chapel Hill - Chapel Hill, NC UNITED STATES - Chapel Hill, NC
Poster Presenter(s)
Introduction: Surgeon decision-making is a key driver of care variation and quality. Despite prior work developing and validating risk prediction tools, uptake in clinical practice remains limited. With broad adoption of electronic health records (EHRs), EHR-based clinical decision support (CDS) offers a potential path forward towards broader uptake. In this context, we assessed urologist attitudes toward EHR-based CDS and explored user preferences and needs.
Methods: We performed an exploratory sequential mixed methods study. Through the 2019 AUA Census survey, we elicited urologist perspectives on the automated calculation and display of validated information on surgical risk and benefits within the EHR at the point-of-care. Next, we interviewed 25 respondents on the potential impact, design preferences, and implementation needs. Bivariable, multivariable, and coding-based thematic analyses were applied, and findings were integrated.
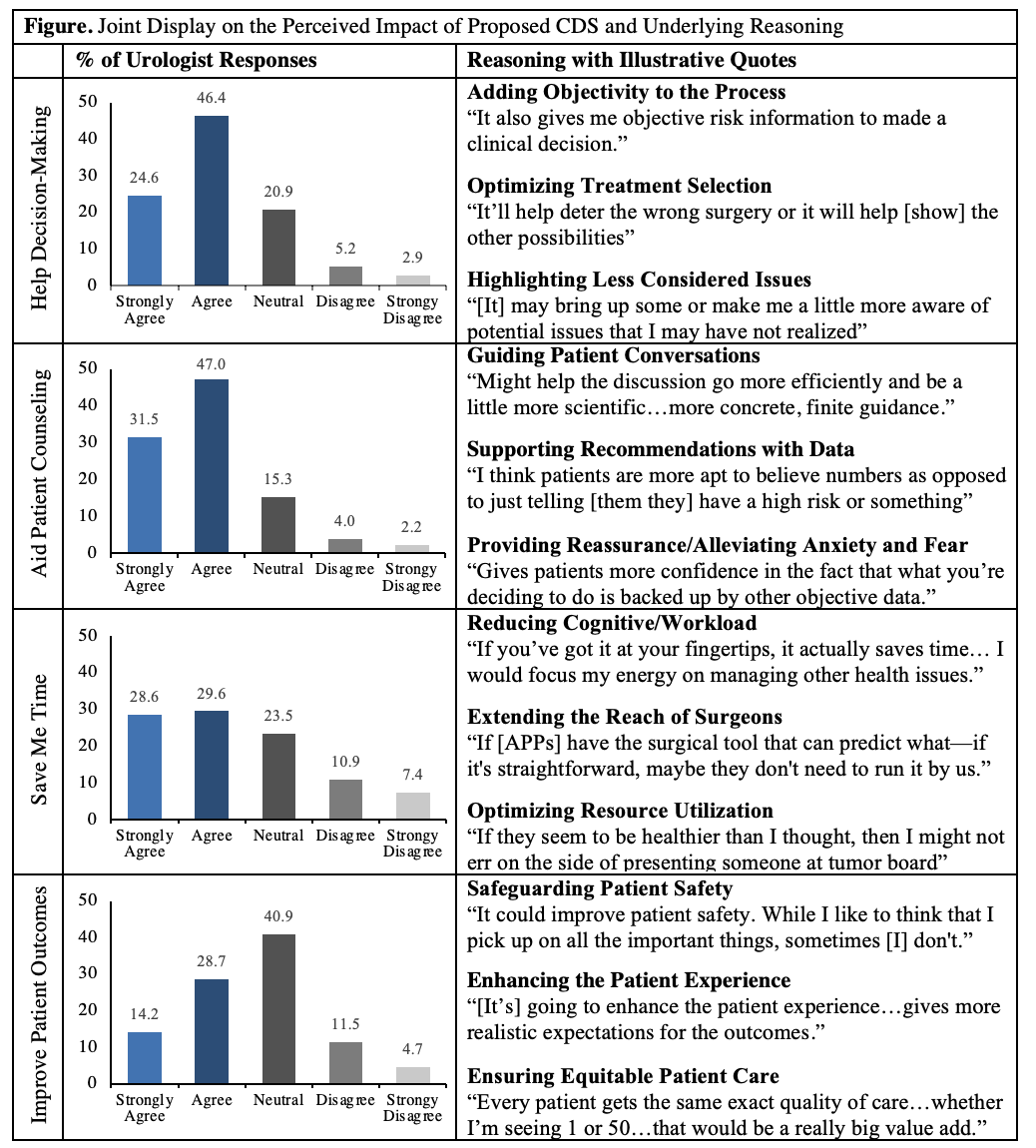
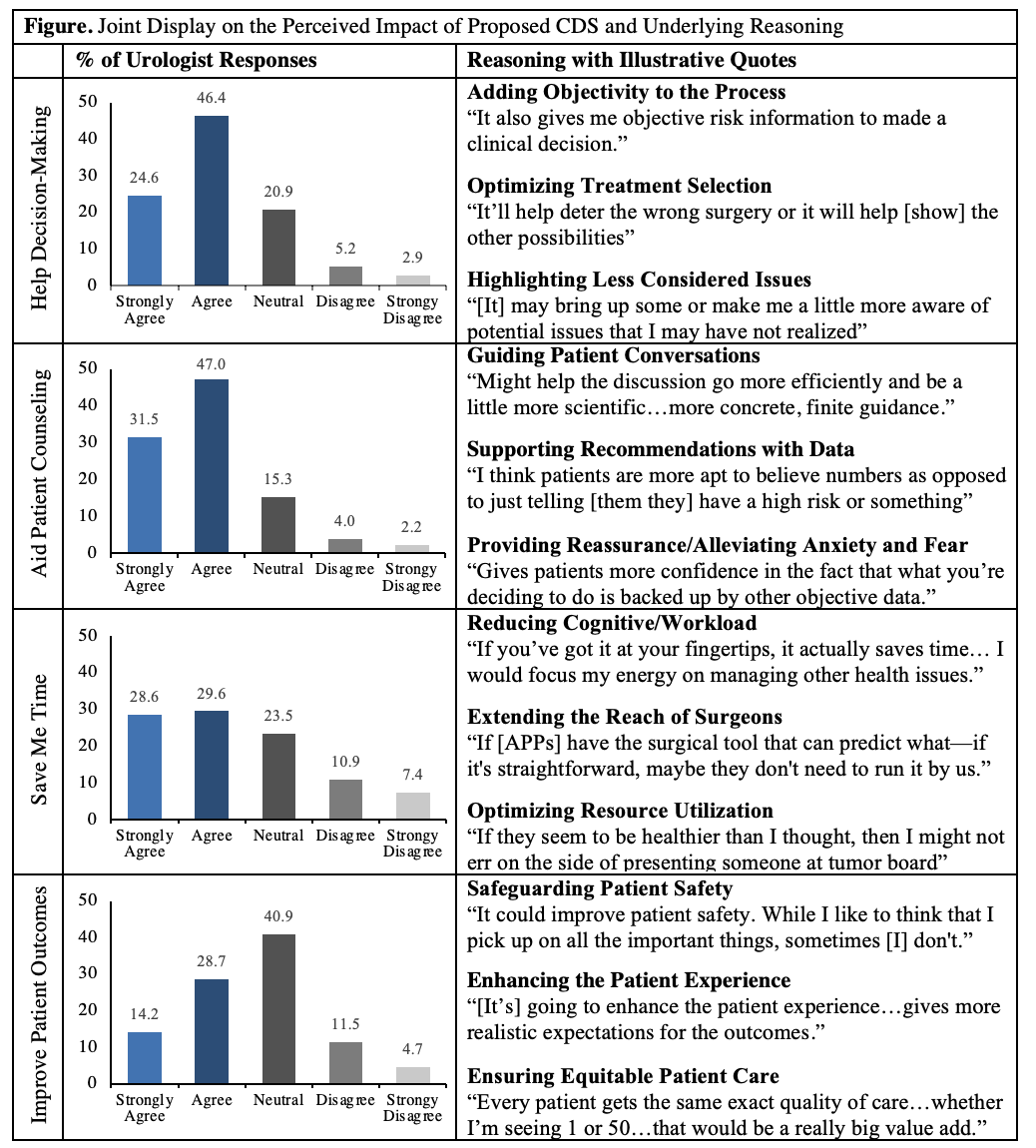
Results: Among a weighted sample of 12,366 urologists, 8,767 (70.9%, CI 68.7-73.2%) agreed that the proposed CDS would help decision-making, 78.5% (CI 76.5-80.5%) agreed it would aid patient counseling, 58.1% (CI 55.7-60.5%) agreed it would save time, and 42.9% (CI 40.5-45.4%) agreed it would improve patient outcomes (Figure). In a multivariable analysis, experience level emerged as the key determinant across all four survey items, with more clinical experience associated with less positive attitudes (p < 0.001). Qualitatively, urologists described multiple ways CDS could help across each domain (Figure). Urologists also offered design features to facilitate ease of use (e.g, automation, prominent location in the EHR, interoperability, familiarity) and usefulness (e.g., customization, patient-facing options, ability to adjust and see outcomes of different choices) as well as implementation strategies to promote uptake (e.g., physician champion, minimal cost, technical support).
Conclusions: Despite the limited impact of risk prediction tools in current practice, urologists expressed favorable attitudes toward the prospect of automating and embedding these tools in the EHR, particularly for supporting decision-making and patient counseling. Based on urologist preferences and needs, user-centered design may increase CDS viability and impact. Models will be developed and tested based on this feedback.
Source of Funding: This work is funded by the Mentored Research Scholar Grant in Applied and Clinical Research, MRSG-18-193-01-CPPB, from the American Cancer Society.
Methods: We performed an exploratory sequential mixed methods study. Through the 2019 AUA Census survey, we elicited urologist perspectives on the automated calculation and display of validated information on surgical risk and benefits within the EHR at the point-of-care. Next, we interviewed 25 respondents on the potential impact, design preferences, and implementation needs. Bivariable, multivariable, and coding-based thematic analyses were applied, and findings were integrated.
Results: Among a weighted sample of 12,366 urologists, 8,767 (70.9%, CI 68.7-73.2%) agreed that the proposed CDS would help decision-making, 78.5% (CI 76.5-80.5%) agreed it would aid patient counseling, 58.1% (CI 55.7-60.5%) agreed it would save time, and 42.9% (CI 40.5-45.4%) agreed it would improve patient outcomes (Figure). In a multivariable analysis, experience level emerged as the key determinant across all four survey items, with more clinical experience associated with less positive attitudes (p < 0.001). Qualitatively, urologists described multiple ways CDS could help across each domain (Figure). Urologists also offered design features to facilitate ease of use (e.g, automation, prominent location in the EHR, interoperability, familiarity) and usefulness (e.g., customization, patient-facing options, ability to adjust and see outcomes of different choices) as well as implementation strategies to promote uptake (e.g., physician champion, minimal cost, technical support).
Conclusions: Despite the limited impact of risk prediction tools in current practice, urologists expressed favorable attitudes toward the prospect of automating and embedding these tools in the EHR, particularly for supporting decision-making and patient counseling. Based on urologist preferences and needs, user-centered design may increase CDS viability and impact. Models will be developed and tested based on this feedback.
Source of Funding: This work is funded by the Mentored Research Scholar Grant in Applied and Clinical Research, MRSG-18-193-01-CPPB, from the American Cancer Society.

.jpg)
.jpg)