Back
Poster, Podium & Video Sessions
Moderated Poster
MP43: Prostate Cancer: Localized: Active Surveillance
MP43-04: Comparison of 4K score, Prostate Health Index, and PSA density in Active Surveillance
Sunday, May 15, 2022
10:30 AM – 11:45 AM
Location: Room 222
Bruce Trock*, Mufaddal Mamawala, Patricia Landis, Yasin Bhanji, Baltimore, MD, Andrew Vickers, New York, NY, Christian Pavlovich, Baltimore, MD
- BT
Bruce J. Trock, PhD
Johns Hopkins School of Medicine
Poster Presenter(s)
Introduction: The 4Kscore combines levels of 4 kallikreins in blood with clinical factors as a measure of the risk of Grade Group [GG]=2 prostate cancer (PCa), while the Prostate Health Index (PHI) measures 3 kallikreins. No previous studies have directly compared the utility of 4Kscore, PHI and PSA density (PSAD) measured in the same men to predict biopsy outcomes on active surveillance (AS). We sought to compare the performance of the 3 biomarkers to predict grade reclassification (GR) to GG=2 in AS men.
Methods: We retrospectively evaluated 133 men with GG1 PCa in Johns Hopkins AS program who had 4Kscore, PHI, and PSA from the same blood sample taken prior to censoring or GR. Multivariable logistic regression was used to predict GR at the next follow-up biopsy (with MRI targeting of any region of interest). Because clinical cutpoints for these biomarkers have not been defined in the AS context, they were modeled as both continuous and dichotomized at the median in non-GR men. The area under the curve (AUC) and likelihood ratio test were used to compare improvement in performance when 4Kscore, PHI, or PSAD were added to a clinical model (age, number of prior biopsies, positive cores and maximum percent cancer in any core at prior biopsy).
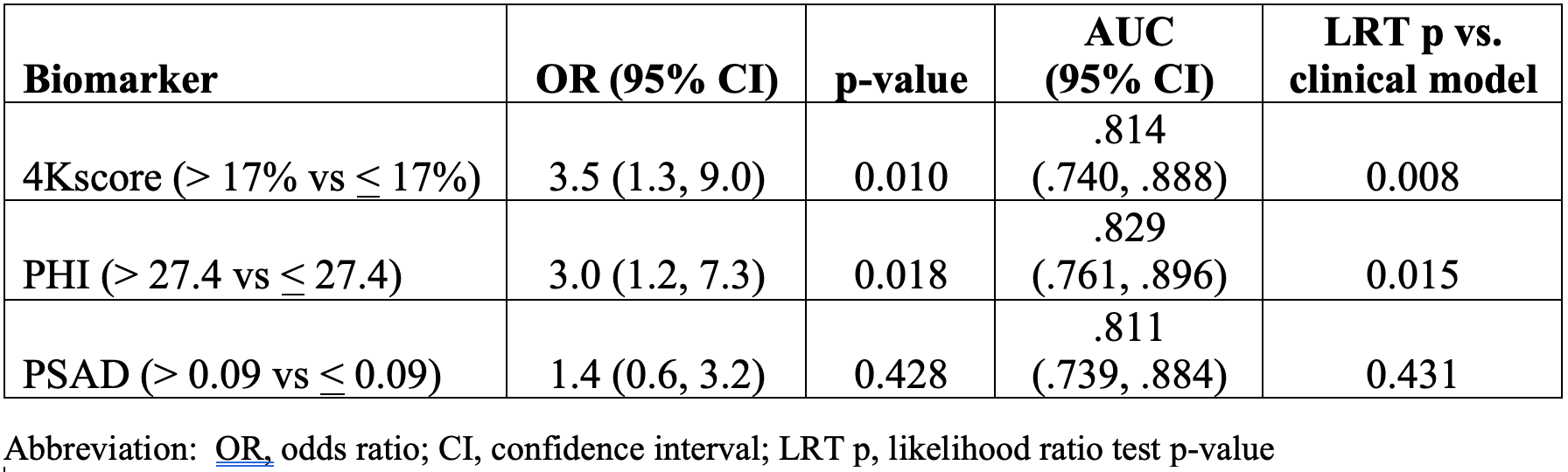
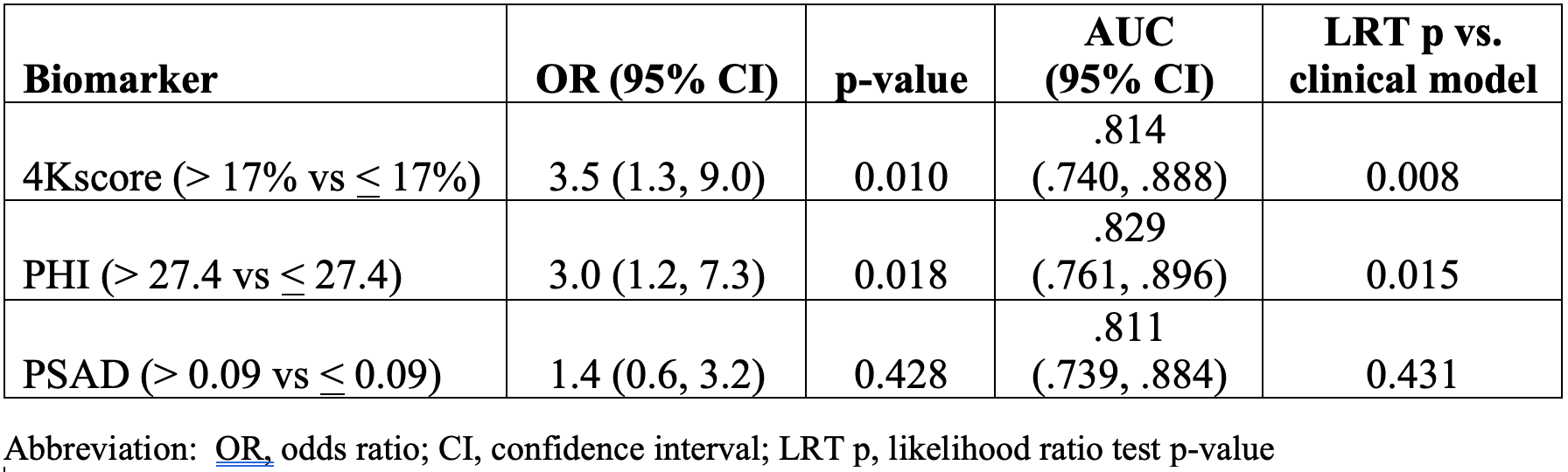
Results: Of 133 men, 56 had GR. The median age at blood draw was 69 (IQR 65–73) with median follow-up 4 years (IQR 2–7). Men with GR had significantly higher PSAD (median 0.13 vs 0.09, p<0.001), PHI (median 37.3 vs 27.4, p<0.001) and 4Kscore (0.33 vs 0.17, p=0.001) compared to men without GR. The AUC of the clinical model was 0.811. As continuous variables none of the biomarkers were significant in the multivariable model, although all slightly increased AUCs: PSAD 0.817; PHI 0.821; 4Kscore 0.815. When dichotomized both PHI and 4Kscore significantly improved model fit vs clinical model (TABLE), and increased AUC: 0.829 and 0.814, respectively.
Conclusions: This is the first direct comparison of 4Kscore and PHI in AS men. They provided minimal improvement in prediction of GR beyond clinical factors in men on AS, with potentially stronger effect when dichotomized. When a clinical model performs so well, biomarkers generally produce small increments in AUC, suggesting potential utility of this clinical model. Larger studies, potentially incorporating MRI findings are needed to determine the clinical utility of these markers in AS.
Source of Funding: James Buchanan Brady Urological Institute
Methods: We retrospectively evaluated 133 men with GG1 PCa in Johns Hopkins AS program who had 4Kscore, PHI, and PSA from the same blood sample taken prior to censoring or GR. Multivariable logistic regression was used to predict GR at the next follow-up biopsy (with MRI targeting of any region of interest). Because clinical cutpoints for these biomarkers have not been defined in the AS context, they were modeled as both continuous and dichotomized at the median in non-GR men. The area under the curve (AUC) and likelihood ratio test were used to compare improvement in performance when 4Kscore, PHI, or PSAD were added to a clinical model (age, number of prior biopsies, positive cores and maximum percent cancer in any core at prior biopsy).
Results: Of 133 men, 56 had GR. The median age at blood draw was 69 (IQR 65–73) with median follow-up 4 years (IQR 2–7). Men with GR had significantly higher PSAD (median 0.13 vs 0.09, p<0.001), PHI (median 37.3 vs 27.4, p<0.001) and 4Kscore (0.33 vs 0.17, p=0.001) compared to men without GR. The AUC of the clinical model was 0.811. As continuous variables none of the biomarkers were significant in the multivariable model, although all slightly increased AUCs: PSAD 0.817; PHI 0.821; 4Kscore 0.815. When dichotomized both PHI and 4Kscore significantly improved model fit vs clinical model (TABLE), and increased AUC: 0.829 and 0.814, respectively.
Conclusions: This is the first direct comparison of 4Kscore and PHI in AS men. They provided minimal improvement in prediction of GR beyond clinical factors in men on AS, with potentially stronger effect when dichotomized. When a clinical model performs so well, biomarkers generally produce small increments in AUC, suggesting potential utility of this clinical model. Larger studies, potentially incorporating MRI findings are needed to determine the clinical utility of these markers in AS.
Source of Funding: James Buchanan Brady Urological Institute

.jpg)
.jpg)