Back
Poster, Podium & Video Sessions
Moderated Poster
MP46: Penile & Testicular Cancer I
MP46-14: Inguinal lymphadenectomy for penile cancer using a fascial sparing technique - outcomes from a single centre
Sunday, May 15, 2022
1:00 PM – 2:15 PM
Location: Room 222
Nicolo' Schifano*, Milan, Italy, Castiglione Fabio, Matthew Rewhorn, Paul Hadway, Rees Rowland, Raj Nigam, Hussain M Alnajjar, Asif Muneer, London, United Kingdom

Nicolo Schifano, MD,MBBS
San Raffaele Hospital
Poster Presenter(s)
Introduction: Radical inguinal lymphadenectomy is performed for penile cancer patients who have pN+ disease in the inguinal lymph nodes. In order to reduce the morbidity, modified approaches have been described to reduce the size of the incision or reduce the number of lymph nodes removed. We describe the technique and report the oncological outcomes and complication rates of a fascial sparing inguinal lymphadenectomy technique.
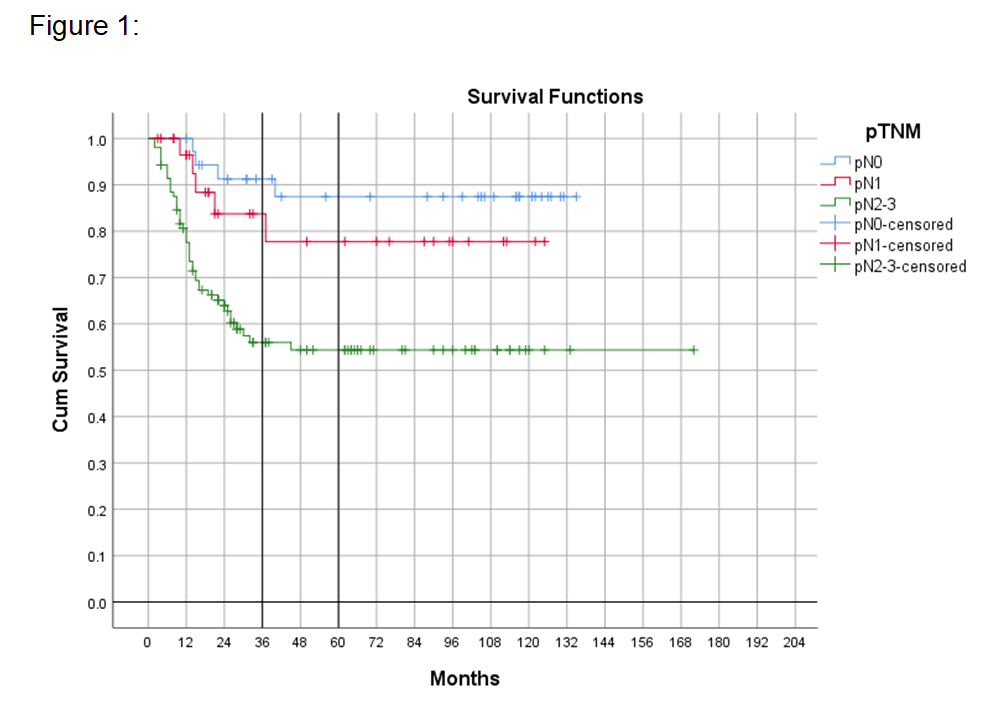
Methods: Over a 10 year period, 294 fascial sparing inguinal lymphadenectomy procedures were performed in 173 patients. The technique uses a subinguinal incision with an ellipse of skin excised if there are any palpable nodes. Identification and preservation of the Scarpa’s and Camper’s fascia is the first layer preserved. All the superficial inguinal nodes were removed en bloc in the femoral triangle under this fascial layer whilst preserving the subcutaneous veins and fascia lata. The saphenous vein was spared where possible as part of the technique. Kaplan-Meier curves estimated the survival functions after the procedure. Postoperative morbidity was also retrospectively analysed.
Results: Median (interquartile range, IQR) follow-up was 28 (14-90) months. A median (IQR) number of 9 (6-12) nodes were removed per groin. The 3-year cancer-specific survival rate was 84% for pN1, and 56% for pN2-3 disease (p < 0.001) compared to 91% for pN0 cases (Figure 1). A total of 105 postoperative complications (35.7%) occurred, including 46 conservatively-managed wound infections (15.6%), 13 cases of deep wound dehiscence (4.4%), 41 cases of lymphoedema (13.9%), 3 cases of deep vein thrombosis (1.0%), 1 case of pulmonary embolism (0.3%), and 1 case of postoperative sepsis (0.3%). There were no patients requiring blood transfusion.
Conclusions: Fascial sparing inguinal dissection offers excellent oncological outcomes whilst decreasing the morbidity rates. Preservation of the fascia lata does not affect oncological outcomes. Patients with more advanced nodal-involvement had poorer survival rates which is in keeping with contemporary data. The technique reduces the risk of wound breakdown and bleeding from the structures deep to the fascia lata.
Source of Funding: No source of founding to be acknowledged.
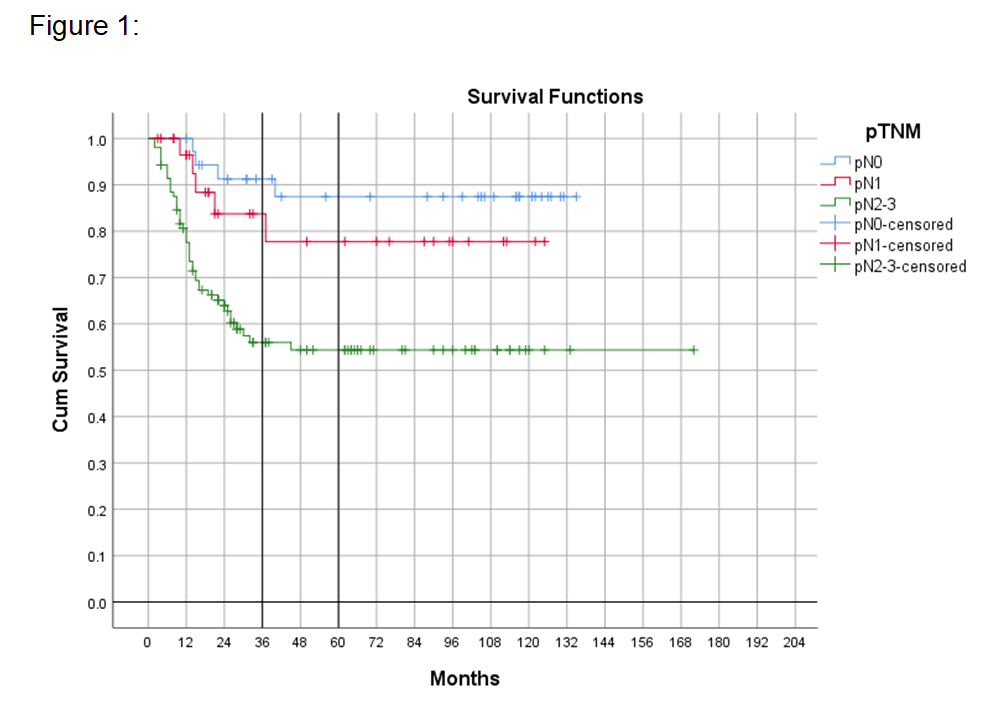
Methods: Over a 10 year period, 294 fascial sparing inguinal lymphadenectomy procedures were performed in 173 patients. The technique uses a subinguinal incision with an ellipse of skin excised if there are any palpable nodes. Identification and preservation of the Scarpa’s and Camper’s fascia is the first layer preserved. All the superficial inguinal nodes were removed en bloc in the femoral triangle under this fascial layer whilst preserving the subcutaneous veins and fascia lata. The saphenous vein was spared where possible as part of the technique. Kaplan-Meier curves estimated the survival functions after the procedure. Postoperative morbidity was also retrospectively analysed.
Results: Median (interquartile range, IQR) follow-up was 28 (14-90) months. A median (IQR) number of 9 (6-12) nodes were removed per groin. The 3-year cancer-specific survival rate was 84% for pN1, and 56% for pN2-3 disease (p < 0.001) compared to 91% for pN0 cases (Figure 1). A total of 105 postoperative complications (35.7%) occurred, including 46 conservatively-managed wound infections (15.6%), 13 cases of deep wound dehiscence (4.4%), 41 cases of lymphoedema (13.9%), 3 cases of deep vein thrombosis (1.0%), 1 case of pulmonary embolism (0.3%), and 1 case of postoperative sepsis (0.3%). There were no patients requiring blood transfusion.
Conclusions: Fascial sparing inguinal dissection offers excellent oncological outcomes whilst decreasing the morbidity rates. Preservation of the fascia lata does not affect oncological outcomes. Patients with more advanced nodal-involvement had poorer survival rates which is in keeping with contemporary data. The technique reduces the risk of wound breakdown and bleeding from the structures deep to the fascia lata.
Source of Funding: No source of founding to be acknowledged.

.jpg)
.jpg)