Back
Poster Session C
Vasculitis
Session: (1543–1578) Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
1573: Von – Willebrand Factor, a Possible Marker for Disease Activity in Vasculitis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- DR
Doron Rimar, MD
Bnai Zion medical center
Haifa, Israel
Abstract Poster Presenter(s)
Jomana mazareeb1, shiri keret1, Abid Awisat1, Itzhak Rosner2, Michel Rozenbaum3, Lisa Kaly1, Gleb Slobodin1 and Doron Rimar1, 1Bnai Zion Medical Center, Haifa, Israel, 2Bnai Zion Medical Center/Technion, Haifa, Israel, 3Bnei Zion Medical Center, Hertzeliya, Israel
Background/Purpose: Vasculitis is an inflammation of blood vessels. While in many cases markers of inflammation as c- reactive protein (CRP) or erythrocytes sedimentation rate (ESR) may correlate with disease activity, in some cases inflammation markers are normal and evaluation of disease activity is based solely on clinical examination or imaging. Von – Willebrand factor (vWF) is a large multimeric glycoprotein, present in peripheral blood. It is produced constitutively as ultra-large VWF in endothelium and subendothelial connective tissue and is packed into storage organelles, the Weibel–Palade bodies (WPBs) on the surface of the endothelium. Damaged endothelium releases vWF. Sporadic reports have suggested vWF to be elevated in vasculitis.
The aim of our study is to evaluate vWF concentration in peripheral blood in patients with vasculitis as a marker of disease activity
Methods: Patients with systemic vasculitis diagnosed by tissue biopsy or typical imaging were classified according to Chapel hill consensus criteria and were evaluated. Demographic characteristics and clinical manifestations were assessed by frontal interview, physical examination and by medical records. Disease activity was reported by BVAS score. VWF was recorded at diagnosis and where available after treatment. vWF antigen was reported in % of predicted value and was adjusted to blood group (vWF level in patients with blood group o is normally reduced by 25% compared to other blood groups)
Results: Twenty-five patients with systemic vasculitis were compared to 15 healthy controls. There was no statistical difference between the two groups regarding age, 56 ± 17 years vs. 48±16 years or sex, females 56% vs. 50% (P=0.54). Forty percent had ANCA-associated vasculitis, 20% had Giant cell arteritis, 16% had polyarteritis nodosa, 8% had Takayasu and the rest had other vasculitides Time from diagnosis was 3.4±5 years. Mean vWF was higher in patients with active vasculitis compared to patients in remission and to healthy controls, 212%±81 vs. 159%±80 vs. 117%±35 p< 0.001 (figure 1) respectively. There was a direct correlation between vWF levels and BVAS score- r=0.31, p=0.04 (figure 2). In 10 patients with active vasculitis, who had a follow-up exam after treatment there was a significant decrease of vWF from 231%±61 to 169%±53 p< 0.02 (figure 3). There was no statistically significant correlation between CRP or ESR to BVAS score, yet CRP correlated directly with vWF r=0.32 p=0.07. In 4 patients who were treated with IL-6 inhibitors, vWF was elevated inspite of normal CRP levels, while clinically vasculitis was active.
Conclusion: This study demonstrates that vWF may be a possible biomarker for disease activity in patients with vasculitis. As vWF reflects direct damage to the endothelium and is not dependent on the IL-6 axis it is not confounded by IL-6 blockers, which are in wide use for vasculitis. Further studies should be undertaken to validate these preliminary findings.
.jpg) graph 1, CRP, ESR and vWF values, in patients with vasculitis, 1A comparison between vWF in patients with active vasculitis, vasculitis patients in remission, and healthy controls. 1B CRP in patients with active vasculitis, vasculitis patients in remission. 1C ESR in patients with active vasculitis compared to vasculitis patients in remission
graph 1, CRP, ESR and vWF values, in patients with vasculitis, 1A comparison between vWF in patients with active vasculitis, vasculitis patients in remission, and healthy controls. 1B CRP in patients with active vasculitis, vasculitis patients in remission. 1C ESR in patients with active vasculitis compared to vasculitis patients in remission
.jpg) Correlation between disease activity according to BVAS and laboratory results. 3A correlation with vWF,
Correlation between disease activity according to BVAS and laboratory results. 3A correlation with vWF,
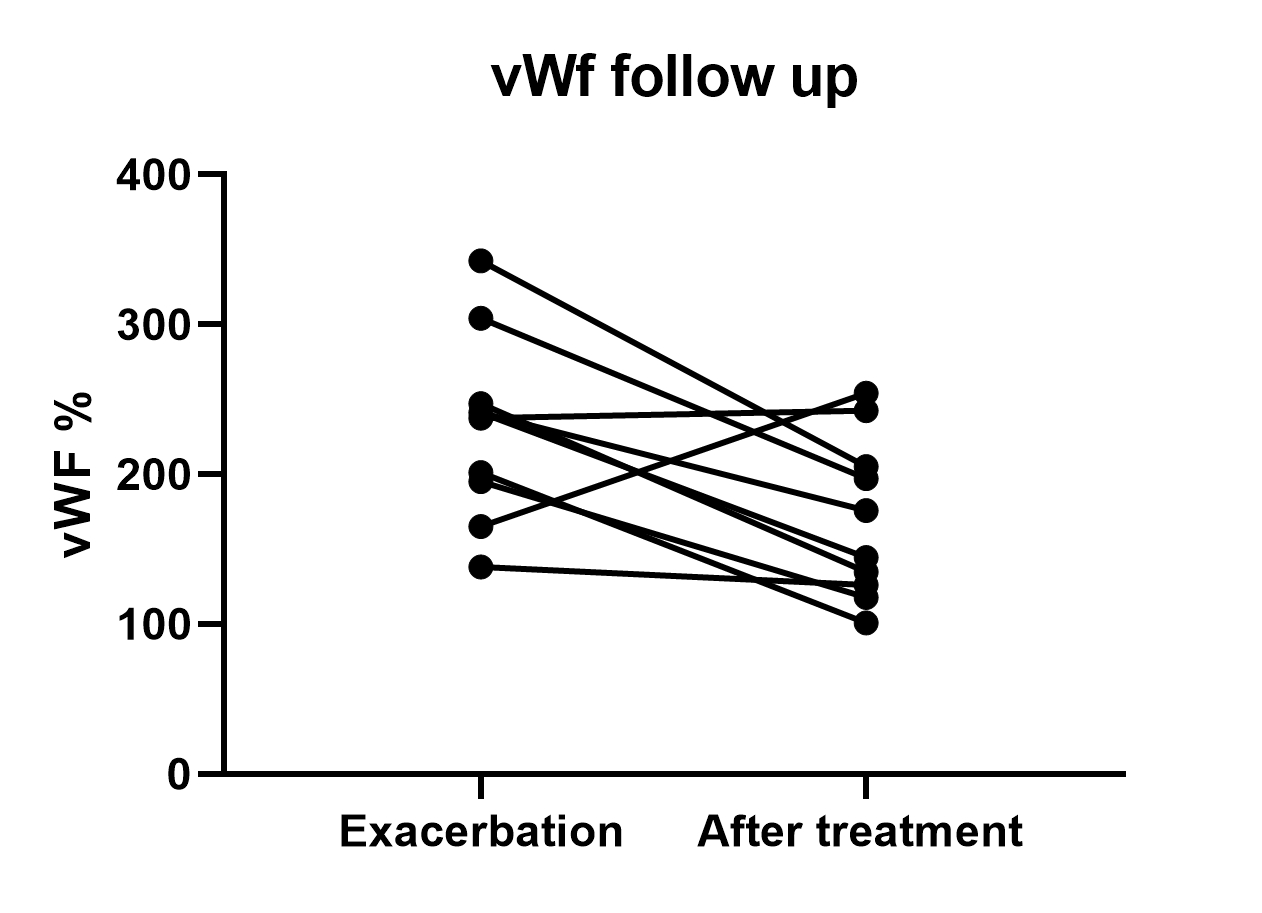 Follow up of vWF in 10 patients with vasculitis once diagnosed and 3-6 months after initiation of treatment.
Follow up of vWF in 10 patients with vasculitis once diagnosed and 3-6 months after initiation of treatment.
Disclosures: J. mazareeb, None; s. keret, None; A. Awisat, None; I. Rosner, None; M. Rozenbaum, None; L. Kaly, None; G. Slobodin, None; D. Rimar, None.
Background/Purpose: Vasculitis is an inflammation of blood vessels. While in many cases markers of inflammation as c- reactive protein (CRP) or erythrocytes sedimentation rate (ESR) may correlate with disease activity, in some cases inflammation markers are normal and evaluation of disease activity is based solely on clinical examination or imaging. Von – Willebrand factor (vWF) is a large multimeric glycoprotein, present in peripheral blood. It is produced constitutively as ultra-large VWF in endothelium and subendothelial connective tissue and is packed into storage organelles, the Weibel–Palade bodies (WPBs) on the surface of the endothelium. Damaged endothelium releases vWF. Sporadic reports have suggested vWF to be elevated in vasculitis.
The aim of our study is to evaluate vWF concentration in peripheral blood in patients with vasculitis as a marker of disease activity
Methods: Patients with systemic vasculitis diagnosed by tissue biopsy or typical imaging were classified according to Chapel hill consensus criteria and were evaluated. Demographic characteristics and clinical manifestations were assessed by frontal interview, physical examination and by medical records. Disease activity was reported by BVAS score. VWF was recorded at diagnosis and where available after treatment. vWF antigen was reported in % of predicted value and was adjusted to blood group (vWF level in patients with blood group o is normally reduced by 25% compared to other blood groups)
Results: Twenty-five patients with systemic vasculitis were compared to 15 healthy controls. There was no statistical difference between the two groups regarding age, 56 ± 17 years vs. 48±16 years or sex, females 56% vs. 50% (P=0.54). Forty percent had ANCA-associated vasculitis, 20% had Giant cell arteritis, 16% had polyarteritis nodosa, 8% had Takayasu and the rest had other vasculitides Time from diagnosis was 3.4±5 years. Mean vWF was higher in patients with active vasculitis compared to patients in remission and to healthy controls, 212%±81 vs. 159%±80 vs. 117%±35 p< 0.001 (figure 1) respectively. There was a direct correlation between vWF levels and BVAS score- r=0.31, p=0.04 (figure 2). In 10 patients with active vasculitis, who had a follow-up exam after treatment there was a significant decrease of vWF from 231%±61 to 169%±53 p< 0.02 (figure 3). There was no statistically significant correlation between CRP or ESR to BVAS score, yet CRP correlated directly with vWF r=0.32 p=0.07. In 4 patients who were treated with IL-6 inhibitors, vWF was elevated inspite of normal CRP levels, while clinically vasculitis was active.
Conclusion: This study demonstrates that vWF may be a possible biomarker for disease activity in patients with vasculitis. As vWF reflects direct damage to the endothelium and is not dependent on the IL-6 axis it is not confounded by IL-6 blockers, which are in wide use for vasculitis. Further studies should be undertaken to validate these preliminary findings.
.jpg) graph 1, CRP, ESR and vWF values, in patients with vasculitis, 1A comparison between vWF in patients with active vasculitis, vasculitis patients in remission, and healthy controls. 1B CRP in patients with active vasculitis, vasculitis patients in remission. 1C ESR in patients with active vasculitis compared to vasculitis patients in remission
graph 1, CRP, ESR and vWF values, in patients with vasculitis, 1A comparison between vWF in patients with active vasculitis, vasculitis patients in remission, and healthy controls. 1B CRP in patients with active vasculitis, vasculitis patients in remission. 1C ESR in patients with active vasculitis compared to vasculitis patients in remission.jpg) Correlation between disease activity according to BVAS and laboratory results. 3A correlation with vWF,
Correlation between disease activity according to BVAS and laboratory results. 3A correlation with vWF,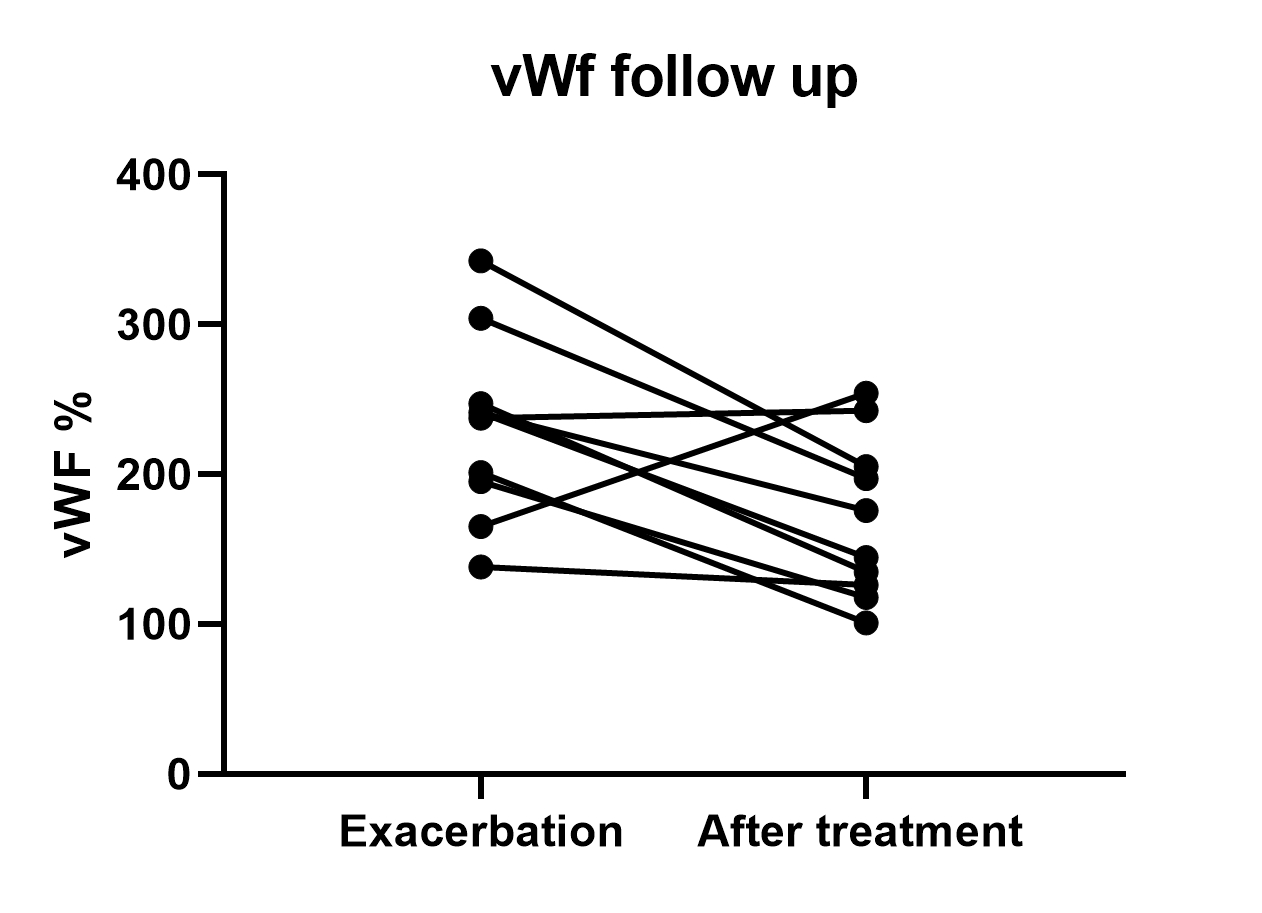 Follow up of vWF in 10 patients with vasculitis once diagnosed and 3-6 months after initiation of treatment.
Follow up of vWF in 10 patients with vasculitis once diagnosed and 3-6 months after initiation of treatment.Disclosures: J. mazareeb, None; s. keret, None; A. Awisat, None; I. Rosner, None; M. Rozenbaum, None; L. Kaly, None; G. Slobodin, None; D. Rimar, None.

