Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0241–0271) RA – Diagnosis, Manifestations, and Outcomes Poster I
0252: Mitochondrial Content in Skeletal Muscle of Individuals with Rheumatoid Arthritis Is Associated with Physical Activity Level
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- BH
Beatriz Hanaoka, MD, MSc
OSU
Columbus, OH, United States
Abstract Poster Presenter(s)
Beatriz Hanaoka1, Jason Benedict1, Guy Brock1, Jillian Johnson1, Peter Reiser1, Kelley Smith-Johnston2, Melissa Sammy3 and Douglas Moellering3, 1The Ohio State University, Columbus, OH, 2University of Alabama at Birmingham, Birmigham, AL, 3University of Alabama at Birmingham, Birmingham, AL
Background/Purpose: Rheumatoid arthritis (RA) is a systemic autoimmune disease associated with a high prevalence of insulin resistance. Skeletal muscle is the major contributor to peripheral insulin resistance. Lower mitochondrial content and/ or mitochondrial oxidative capacity have been reported in skeletal muscle of individuals with obesity or type2 diabetes mellitus. Our goal was to investigate mitochondrial content and function in skeletal muscle of patients with RA and to explore associations of mitochondrial content with factors involved in mitochondrial biogenesis (insulin resistance, age, physical activity and inflammation). We hypothesized that insulin resistance is associated with mitochondrial dysfunction in RA patients.
Methods: This was a prospective, cross-sectional study. 24 RA subjects between 35-65 years who met the 2010 ACR /EULAR criteria for RA, and 20 healthy individuals were enrolled as controls. Physical activity level was assessed by self-report (IPAQ long form) and accelerometer (wGT3X-BT, ActiGraph, Pensacola, FL). Citrate synthase activity (CSA) and mitochondrial complex IV activity (subsarcolemmal and intermyofibrillary mitochondrial subpopulations) in biopsy samples of the vastus lateralis muscle were used as validated biomarkers for skeletal muscle mitochondrial density and oxidative capacity (OXPHOS), respectively. Insulin resistance was estimated using the homeostasis model assessment of insulin resistance (HOMA-IR) index. RA activity was assessed using the DAS28-CRP score. Body composition [fat mass index (FMI) and fat free mass index (FFMI)] was assessed by DXA (GE-Lunar Radiation Corp. Madison, WI). Spearman's rank correlation was calculated to assess correlations between variables of interest.
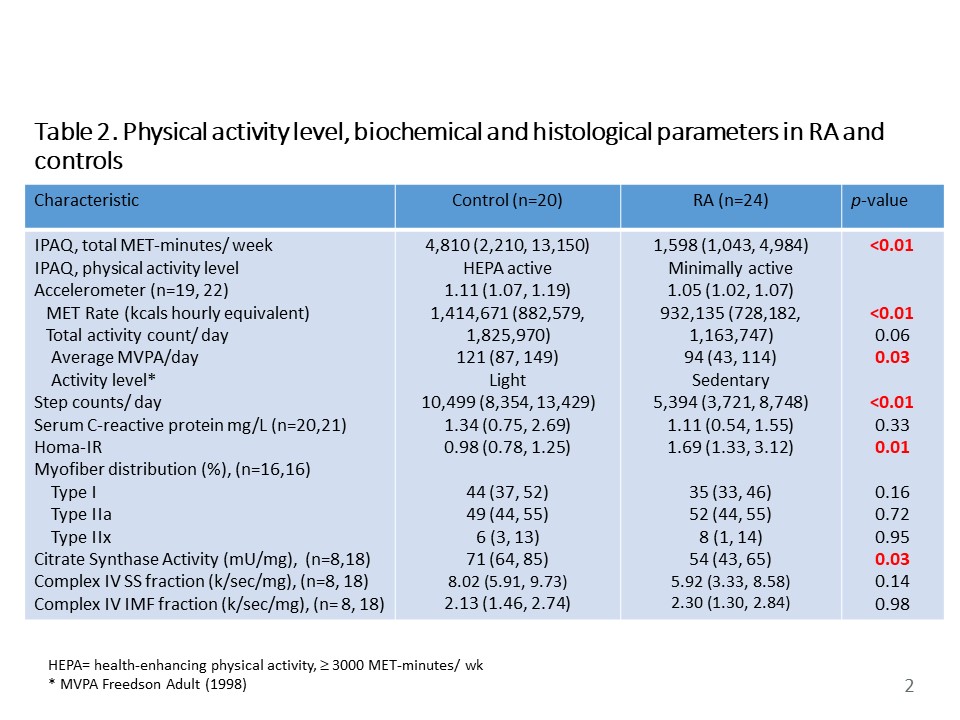
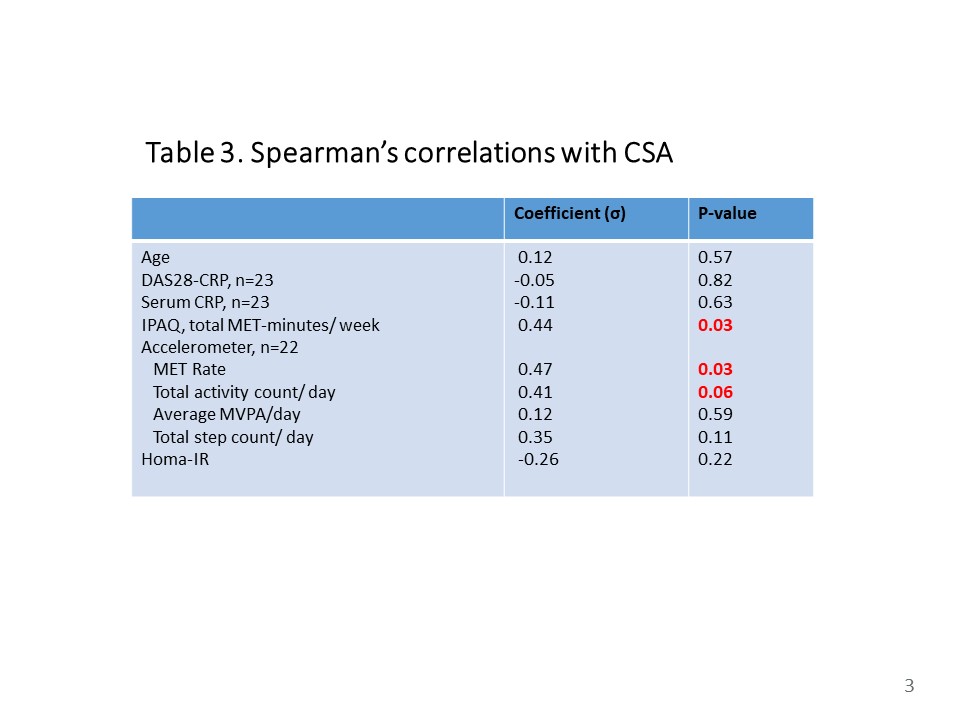
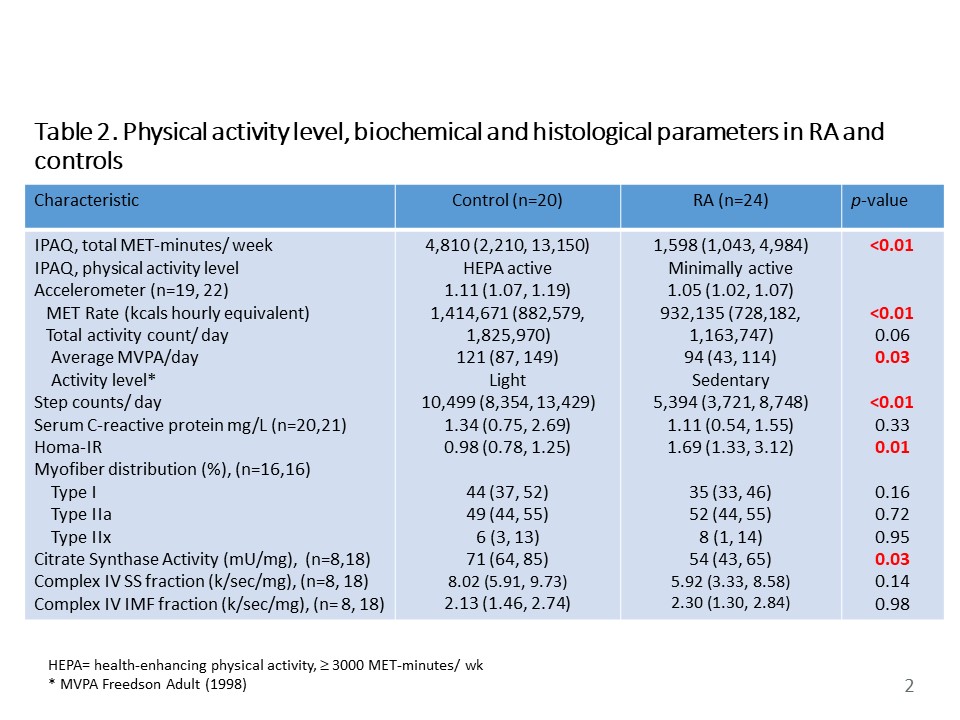
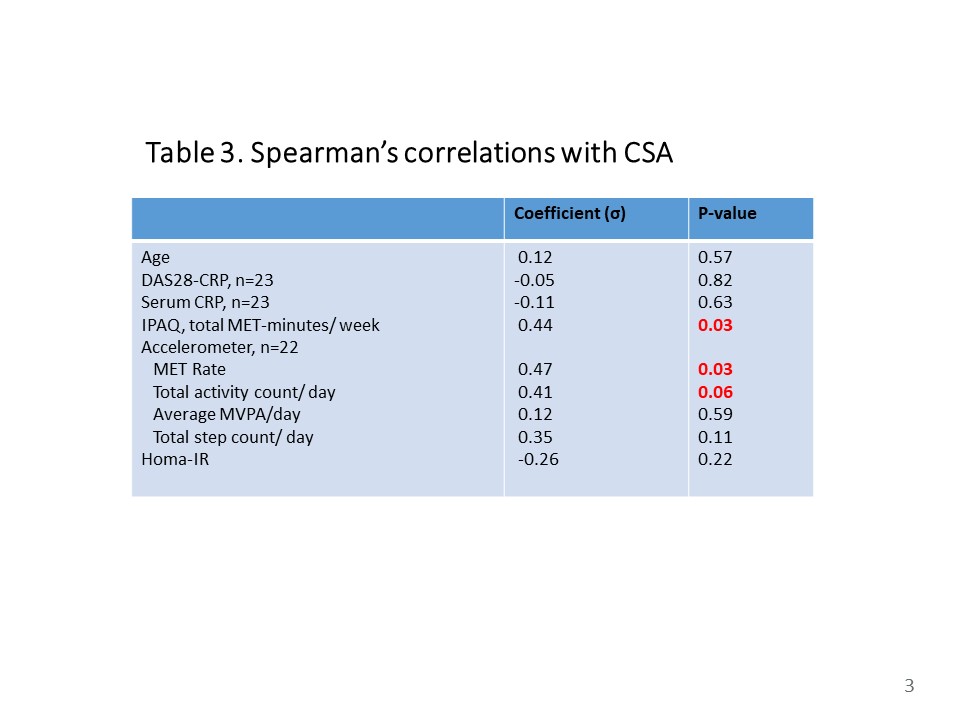
Results: RA subjects and controls were not significantly different in age, sex, anthropometric measures (body mass index, waist-to-hip circumference), myofiber distribution, body composition or serum CRP (Table1). Among the RA subjects, the median DAS28-CRP was 1.77 (1.23, 3.13), 94% of subjects were on at least one Disease-Modifying Antirheumatic Drug (DMARD) and only 13% of subjects were currently on prednisone with a median dose of 5 mg/ day (IQR=5,5). Despite adequate disease control, RA subjects had significantly lower physical activity measures [IPAQ total MET-minutes/ week (p< 0.01), MET Rate (p< 0.01), average MVPA/ day (p=0.03) and step counts/day (p< 0.01)] and higher HOMA-IR compared to controls (p< 0.01) (Table 2). CSA, but not Complex IV activity, was significantly lower in RA vs. controls (p=0.03) (Table 2). CSA was significantly correlated with IPAQ, total MET-minutes/ week (p=0.03) and MET rate (p=0.03) among RA subjects (Table 3).
Conclusion: Lower skeletal muscle CSA among RA subjects suggests patients with RA could have lower skeletal muscle mitochondrial content. CSA was positively correlated with measures of physical activity among RA subjects, highlighting the importance of physical activity in RA. Complex IV activity was not statistically different between RA subjects and controls, suggesting that mitochondrial oxidative function is preserved in RA.
.jpg)
Disclosures: B. Hanaoka, None; J. Benedict, None; G. Brock, None; J. Johnson, None; P. Reiser, None; K. Smith-Johnston, None; M. Sammy, None; D. Moellering, None.
Background/Purpose: Rheumatoid arthritis (RA) is a systemic autoimmune disease associated with a high prevalence of insulin resistance. Skeletal muscle is the major contributor to peripheral insulin resistance. Lower mitochondrial content and/ or mitochondrial oxidative capacity have been reported in skeletal muscle of individuals with obesity or type2 diabetes mellitus. Our goal was to investigate mitochondrial content and function in skeletal muscle of patients with RA and to explore associations of mitochondrial content with factors involved in mitochondrial biogenesis (insulin resistance, age, physical activity and inflammation). We hypothesized that insulin resistance is associated with mitochondrial dysfunction in RA patients.
Methods: This was a prospective, cross-sectional study. 24 RA subjects between 35-65 years who met the 2010 ACR /EULAR criteria for RA, and 20 healthy individuals were enrolled as controls. Physical activity level was assessed by self-report (IPAQ long form) and accelerometer (wGT3X-BT, ActiGraph, Pensacola, FL). Citrate synthase activity (CSA) and mitochondrial complex IV activity (subsarcolemmal and intermyofibrillary mitochondrial subpopulations) in biopsy samples of the vastus lateralis muscle were used as validated biomarkers for skeletal muscle mitochondrial density and oxidative capacity (OXPHOS), respectively. Insulin resistance was estimated using the homeostasis model assessment of insulin resistance (HOMA-IR) index. RA activity was assessed using the DAS28-CRP score. Body composition [fat mass index (FMI) and fat free mass index (FFMI)] was assessed by DXA (GE-Lunar Radiation Corp. Madison, WI). Spearman's rank correlation was calculated to assess correlations between variables of interest.
Results: RA subjects and controls were not significantly different in age, sex, anthropometric measures (body mass index, waist-to-hip circumference), myofiber distribution, body composition or serum CRP (Table1). Among the RA subjects, the median DAS28-CRP was 1.77 (1.23, 3.13), 94% of subjects were on at least one Disease-Modifying Antirheumatic Drug (DMARD) and only 13% of subjects were currently on prednisone with a median dose of 5 mg/ day (IQR=5,5). Despite adequate disease control, RA subjects had significantly lower physical activity measures [IPAQ total MET-minutes/ week (p< 0.01), MET Rate (p< 0.01), average MVPA/ day (p=0.03) and step counts/day (p< 0.01)] and higher HOMA-IR compared to controls (p< 0.01) (Table 2). CSA, but not Complex IV activity, was significantly lower in RA vs. controls (p=0.03) (Table 2). CSA was significantly correlated with IPAQ, total MET-minutes/ week (p=0.03) and MET rate (p=0.03) among RA subjects (Table 3).
Conclusion: Lower skeletal muscle CSA among RA subjects suggests patients with RA could have lower skeletal muscle mitochondrial content. CSA was positively correlated with measures of physical activity among RA subjects, highlighting the importance of physical activity in RA. Complex IV activity was not statistically different between RA subjects and controls, suggesting that mitochondrial oxidative function is preserved in RA.
.jpg)
Disclosures: B. Hanaoka, None; J. Benedict, None; G. Brock, None; J. Johnson, None; P. Reiser, None; K. Smith-Johnston, None; M. Sammy, None; D. Moellering, None.

