Back
Poster Session A
Patient engagement/self-management
Session: (PP01–PP22) Patient Perspectives Poster
PP16: Please Hear Me: How Effective Provider-Patient Communication Improved My Psoriatic Arthritis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AK
Ashley Krivohlavek, MA
Self-employed
Claremore, OK, United StatesDisclosure: Disclosure(s): No financial relationships to disclose
Patient Poster Presenter(s)
Ashley Krivohlavek, Oklahoma City, OK
Background/Purpose: At age 12, I was diagnosed with psoriasis (PsO) followed by a diagnosis of psoriatic arthritis (PsA) at age 30. I'm now 38.
In 2020, I had been on an infused biologic for 18 months, but my dose was wearing off between infusions. My disease activity was worsening, and my CRP kept going up. My rheumatologist recommended an injectable. I started the new medication in spring; by summer I was miserable. I had pain, swelling, fatigue, and brain fog. This meant I was unable to do basic activities like laundry, cooking, or even walking.
At the end of August, I asked my provider for a new medication. I was met with no sense of collaboration. She said there was no reason for my worsening symptoms and that it may be fibromyalgia. I left that appointment feeling dismayed by the lack of collaboration and hopeless at the prospect of managing an added diagnosis.
Intervention: I started researching. I Googled medical studies and articles about PsA with fibromyalgia and medications. I discovered that PsA and fibromyalgia are comorbidities and that switching biologics can cause flares. What I was experiencing aligned with symptoms of uncontrolled PsA with a few overlapping fibromyalgia symptoms.
I also looked for other rheumatologists. I consulted with the Dean of Rheumatology at my state university who confirmed that I was not a candidate for fibromyalgia. My symptoms were likely due to uncontrolled PsA. She gave me the name of another rheumatologist, who also confirmed the same.
In a rheumatology desert, with few options, I thought I might have to travel out of state. Fortunately, I stumbled on a practice new to my area that employed nurse practitioners with rheumatology specialization and made an appointment. The first thing my new provider said was that she expected me to be a collaborator in my health journey. I was the captain of my ship, and she was there to support me. She read my notes prior to our visit and ordered extensive labs. We scheduled a follow-up to review my labs and discuss next steps. I felt understood and hopeful.
Maintenance: Since 2021, my health has improved. Gone is the constant fatigue and brain fog and aching swollen joints. My CRP levels are lower than they've been since my PsA diagnosis.
Quality of Life: My life has become my own again. I re-started graduate school and have been volunteering in health advocacy in my state. The time and effort that goes into having a chronic illness has also become less burdensome: I don't need to travel to doctor's appointments as often and I spend less time on the phone with my doctor's office and insurance company.
This has all been possible because of the collaborative relationship I now have with my rheumatology provider. I communicate with my provider about my needs and PsA goals and she listens and provides constructive feedback. To maintain our collaborative relationship, I wrote up patient communication principles based on my experience (Table 1). If I need to change my provider again in the future, I know I can do so with confidence using my Guide to Changing Providers (Figure 1).
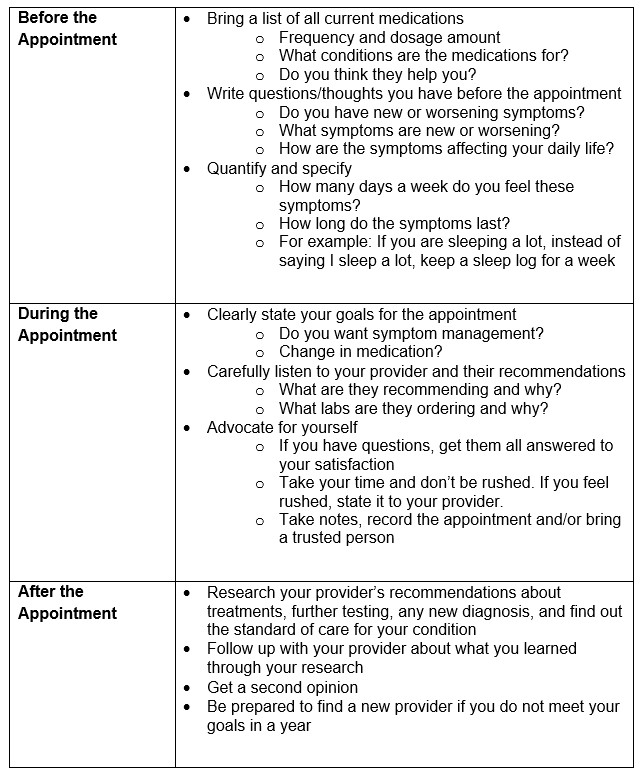 Table 1. Guide to Collaborating with Your Provider
Table 1. Guide to Collaborating with Your Provider
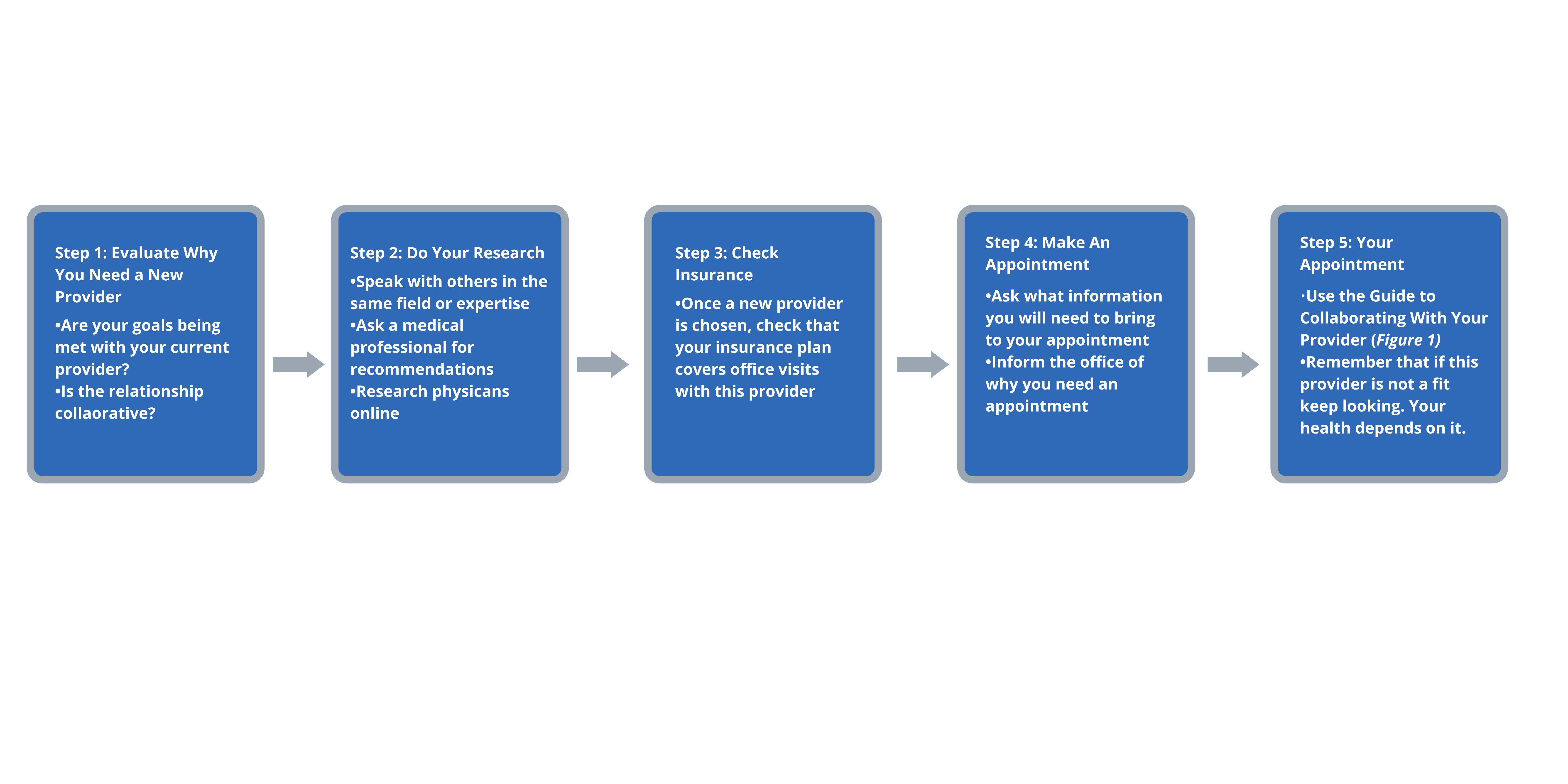 Figure 1. Guide to Changing Providers
Figure 1. Guide to Changing Providers
Disclosures: A. Krivohlavek, None.
Background/Purpose: At age 12, I was diagnosed with psoriasis (PsO) followed by a diagnosis of psoriatic arthritis (PsA) at age 30. I'm now 38.
In 2020, I had been on an infused biologic for 18 months, but my dose was wearing off between infusions. My disease activity was worsening, and my CRP kept going up. My rheumatologist recommended an injectable. I started the new medication in spring; by summer I was miserable. I had pain, swelling, fatigue, and brain fog. This meant I was unable to do basic activities like laundry, cooking, or even walking.
At the end of August, I asked my provider for a new medication. I was met with no sense of collaboration. She said there was no reason for my worsening symptoms and that it may be fibromyalgia. I left that appointment feeling dismayed by the lack of collaboration and hopeless at the prospect of managing an added diagnosis.
Intervention: I started researching. I Googled medical studies and articles about PsA with fibromyalgia and medications. I discovered that PsA and fibromyalgia are comorbidities and that switching biologics can cause flares. What I was experiencing aligned with symptoms of uncontrolled PsA with a few overlapping fibromyalgia symptoms.
I also looked for other rheumatologists. I consulted with the Dean of Rheumatology at my state university who confirmed that I was not a candidate for fibromyalgia. My symptoms were likely due to uncontrolled PsA. She gave me the name of another rheumatologist, who also confirmed the same.
In a rheumatology desert, with few options, I thought I might have to travel out of state. Fortunately, I stumbled on a practice new to my area that employed nurse practitioners with rheumatology specialization and made an appointment. The first thing my new provider said was that she expected me to be a collaborator in my health journey. I was the captain of my ship, and she was there to support me. She read my notes prior to our visit and ordered extensive labs. We scheduled a follow-up to review my labs and discuss next steps. I felt understood and hopeful.
Maintenance: Since 2021, my health has improved. Gone is the constant fatigue and brain fog and aching swollen joints. My CRP levels are lower than they've been since my PsA diagnosis.
Quality of Life: My life has become my own again. I re-started graduate school and have been volunteering in health advocacy in my state. The time and effort that goes into having a chronic illness has also become less burdensome: I don't need to travel to doctor's appointments as often and I spend less time on the phone with my doctor's office and insurance company.
This has all been possible because of the collaborative relationship I now have with my rheumatology provider. I communicate with my provider about my needs and PsA goals and she listens and provides constructive feedback. To maintain our collaborative relationship, I wrote up patient communication principles based on my experience (Table 1). If I need to change my provider again in the future, I know I can do so with confidence using my Guide to Changing Providers (Figure 1).
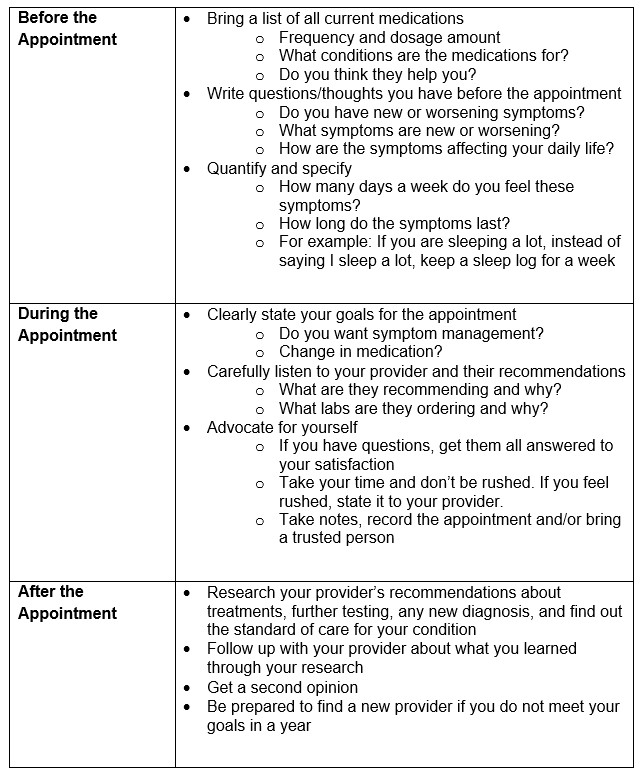 Table 1. Guide to Collaborating with Your Provider
Table 1. Guide to Collaborating with Your Provider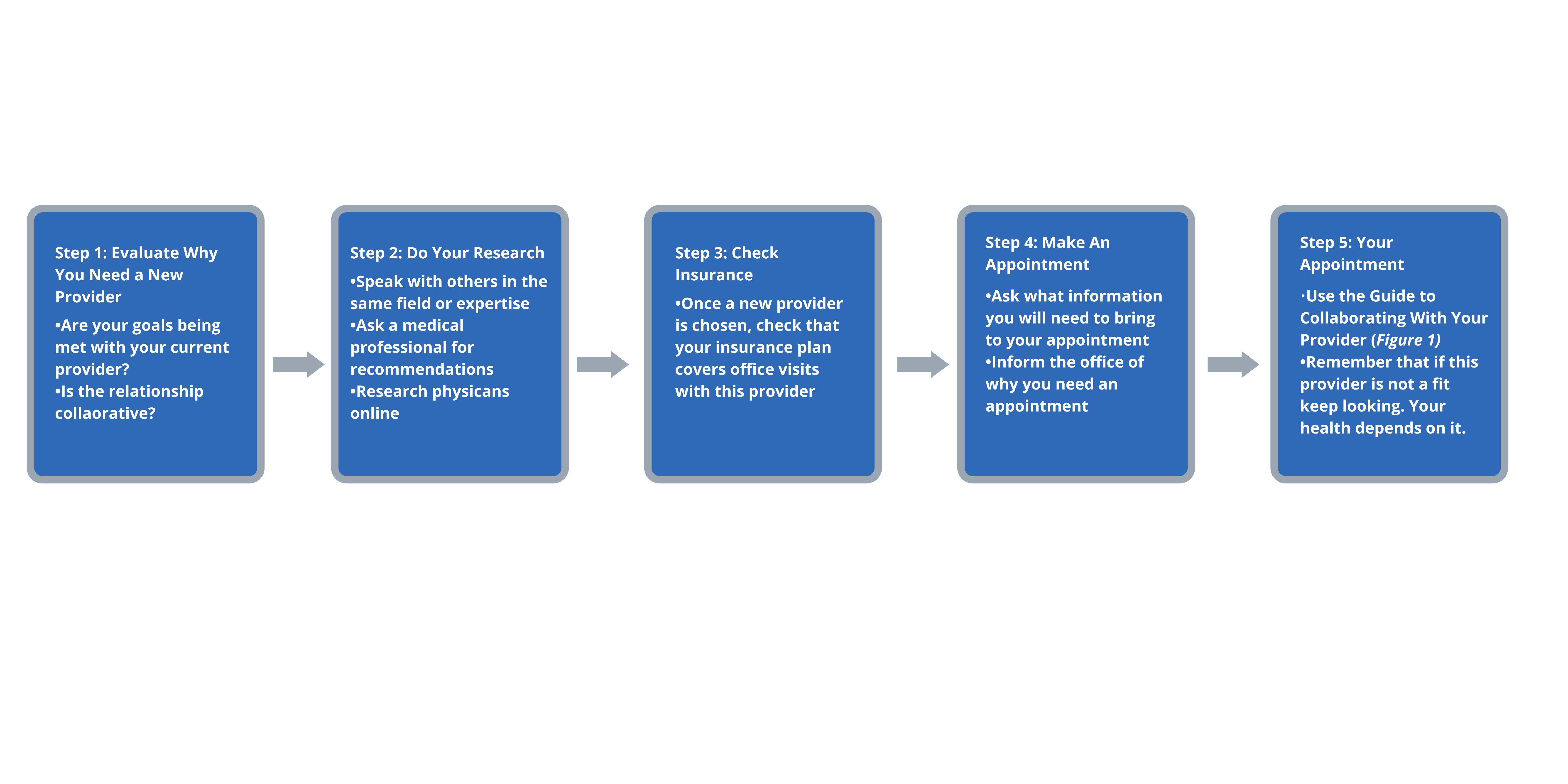 Figure 1. Guide to Changing Providers
Figure 1. Guide to Changing ProvidersDisclosures: A. Krivohlavek, None.

