Back
Plenary Session
Epidemiology, health policy and outcomes
Session: Plenary II
1115: Medication Co-pay Modifies Treatment Adherence in Patients with Systemic Lupus Erythematosus
Sunday, November 13, 2022
12:15 PM – 12:25 PM Eastern Time
Location: Exhibit Hall A
- RL
Raisa Lomanto Silva, MD
University of Pittsburgh Medical Center
Pittsburgh, PA, United States
Presenting Author(s)
Raisa Lomanto Silva1, Gretchen M Swabe2 and Jared W Magnani3, 1University of Pittsburgh Medical Center, Pittsburgh, PA, 2Division of Cardiology, University of Pittsburgh School of Medicine, Pittsburgh, PA, 3Heart and Vascular Institute, University of Pittsburgh Medical Center; Division of Cardiology, University of Pittsburgh School of Medicine, Pittsburgh, PA
Background/Purpose: Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease with significant morbidity and mortality. Adherence to SLE medications is challenging and estimated as 30-80% for prescribed therapies. Hydroxychloroquine, the backbone of SLE treatment, has been associated with very poor adherence. Multiple social factors may affect treatment adherence. The costs of insurance copayment, or copays, may represent a major obstacle to adherence, particularly for individuals with limited social resources. We investigate the association between SLE medications co-pay and adherence.
Methods: We used an administrative claims dataset (Optum's de-identified Clinformatics® Data Mart Database) to identify individuals with incident SLE diagnosis (defined as 2 ICD-9/10 codes within 30 days) between 2010-19 receiving hydroxychloroquine (HCQ), azathioprine (AZA), or mycophenolate mofetil (MMF) and at least 90 days of medication claims data. We dichotomized copays into low (<$10/30 days) and high (≥$10/30 days). We examined the association between medication copay and odds of adherence in multivariable-adjusted regression models. Adherence was defined as proportion of days covered (PDC) ≥80%. We adjusted for demographics, comorbid conditions, and socioeconomic factors including annual household income and educational attainment.
Results: We identified 12510 individuals (age 54.2±15.5; 88.2% women; 14.9% Black race), of whom 9510 (76%) were on HCQ and 15% on HCQ and another medication. Median (IQR) 30-day copays were $8 (4, 10) for HCQ, $7 (2, 10) for AZA, and $10 (5, 20) for MMF. We identified significant associations between higher copays and lower adherence. In our fully adjusted model, high copays were associated with 39% (95% CI, 0.55-0.68) lower odds of adherence for HCQ; 56% (95% CI, 0.29-0.65) lower odds of adherence for AZA; and 32% (95% CI 0.49-0.96) lower odds of adherence for MMF.
Conclusion: In a large, administrative health claims database we identified that increased copays are associated with reduced adherence to the most commonly used medications for SLE. Incorporating awareness of the burden of copayments and their consequences into health care practice is essential for improving medication access in individuals with this complex condition.
.jpg) Graph 1. Odds Ratio of Adherence by Medication Class adjusted for Demographics and Socioeconomic Factors
Graph 1. Odds Ratio of Adherence by Medication Class adjusted for Demographics and Socioeconomic Factors
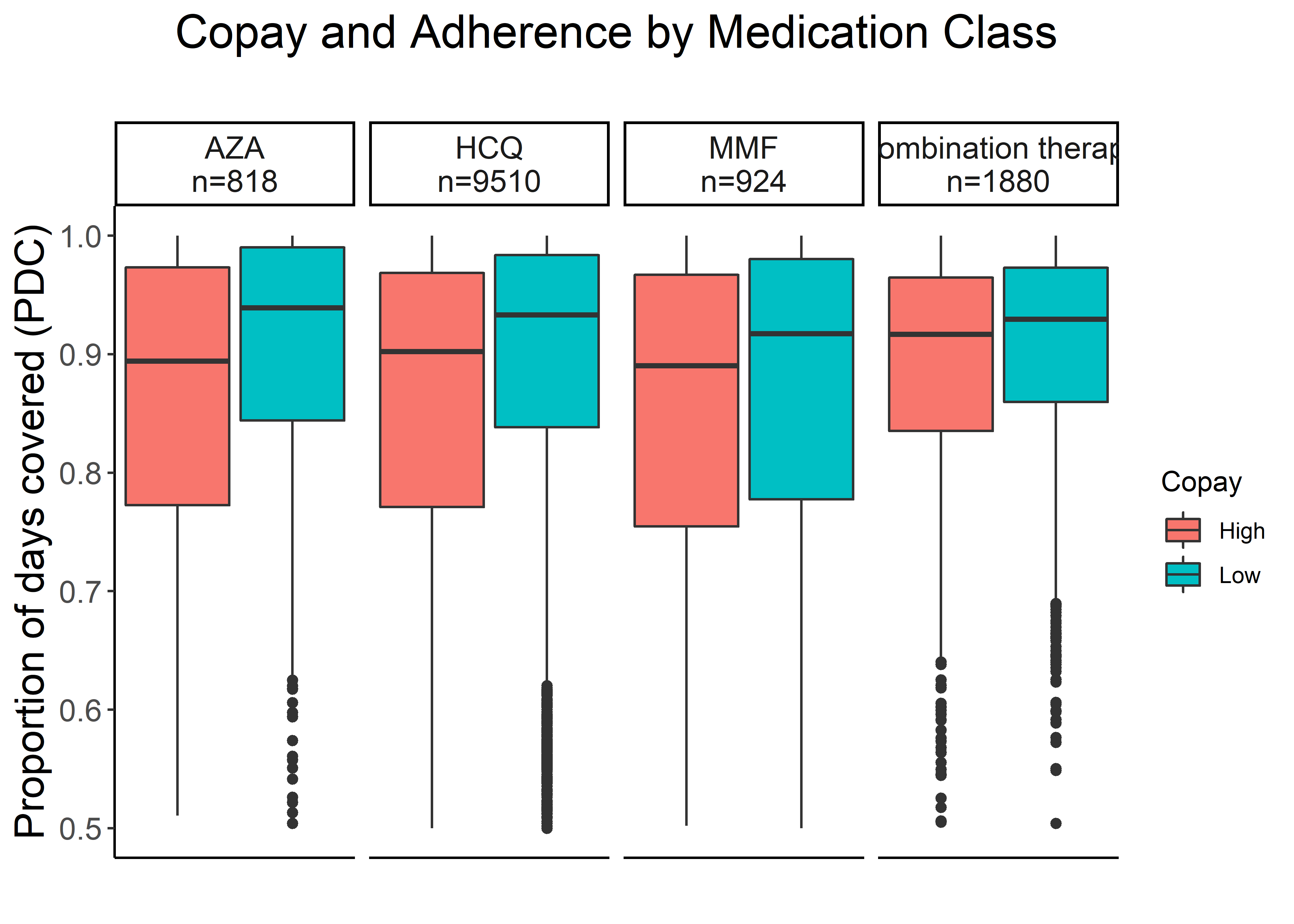 Graph 2. Copay and Adherence (Proportion of Days Covered) per Medication Class
Graph 2. Copay and Adherence (Proportion of Days Covered) per Medication Class
Disclosures: R. Lomanto Silva, None; G. M Swabe, None; J. W Magnani, None.
Background/Purpose: Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease with significant morbidity and mortality. Adherence to SLE medications is challenging and estimated as 30-80% for prescribed therapies. Hydroxychloroquine, the backbone of SLE treatment, has been associated with very poor adherence. Multiple social factors may affect treatment adherence. The costs of insurance copayment, or copays, may represent a major obstacle to adherence, particularly for individuals with limited social resources. We investigate the association between SLE medications co-pay and adherence.
Methods: We used an administrative claims dataset (Optum's de-identified Clinformatics® Data Mart Database) to identify individuals with incident SLE diagnosis (defined as 2 ICD-9/10 codes within 30 days) between 2010-19 receiving hydroxychloroquine (HCQ), azathioprine (AZA), or mycophenolate mofetil (MMF) and at least 90 days of medication claims data. We dichotomized copays into low (<$10/30 days) and high (≥$10/30 days). We examined the association between medication copay and odds of adherence in multivariable-adjusted regression models. Adherence was defined as proportion of days covered (PDC) ≥80%. We adjusted for demographics, comorbid conditions, and socioeconomic factors including annual household income and educational attainment.
Results: We identified 12510 individuals (age 54.2±15.5; 88.2% women; 14.9% Black race), of whom 9510 (76%) were on HCQ and 15% on HCQ and another medication. Median (IQR) 30-day copays were $8 (4, 10) for HCQ, $7 (2, 10) for AZA, and $10 (5, 20) for MMF. We identified significant associations between higher copays and lower adherence. In our fully adjusted model, high copays were associated with 39% (95% CI, 0.55-0.68) lower odds of adherence for HCQ; 56% (95% CI, 0.29-0.65) lower odds of adherence for AZA; and 32% (95% CI 0.49-0.96) lower odds of adherence for MMF.
Conclusion: In a large, administrative health claims database we identified that increased copays are associated with reduced adherence to the most commonly used medications for SLE. Incorporating awareness of the burden of copayments and their consequences into health care practice is essential for improving medication access in individuals with this complex condition.
.jpg) Graph 1. Odds Ratio of Adherence by Medication Class adjusted for Demographics and Socioeconomic Factors
Graph 1. Odds Ratio of Adherence by Medication Class adjusted for Demographics and Socioeconomic Factors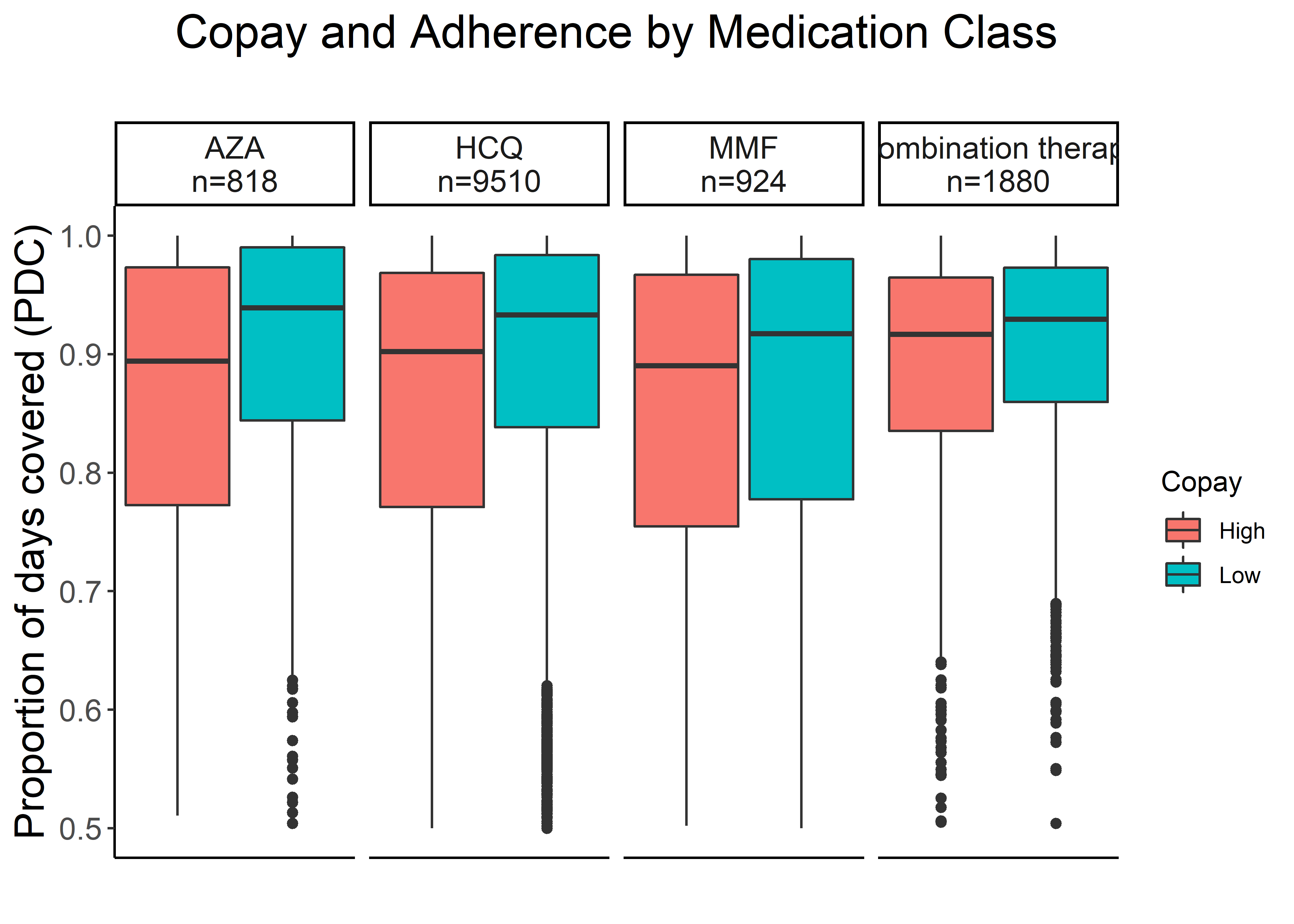 Graph 2. Copay and Adherence (Proportion of Days Covered) per Medication Class
Graph 2. Copay and Adherence (Proportion of Days Covered) per Medication ClassDisclosures: R. Lomanto Silva, None; G. M Swabe, None; J. W Magnani, None.

