Back
Abstract Session
Epidemiology, health policy and outcomes
Session: Abstracts: Epidemiology and Public Health I: Risk Factors and Outcomes (1633–1638)
1634: Association of Ultra-processed Food Intake with Risk of Systemic Lupus Erythematosus in Women
Monday, November 14, 2022
9:15 AM – 9:25 AM Eastern Time
Location: Room 204

Karen Costenbader, MD, MPH
Brigham and Women's Hospital/ Harvard Medical School
BOSTON, MA, United States
Presenting Author(s)
Sinara Laurini Rossato1, Chun-Han Lo2, Medha Barbhaiya3, Jeffrey Sparks4, Neha Khandpur5, Susan Malspeis6, Kazuki Yoshida6, Walter C. Willett7 and Karen Costenbader6, 1Universidade Federal de Uberlândia, Uberlândia, Brazil, 2Kirk Kerkorian School of Medicine at UNLV, Las Vegas, 3Hospital for Special Surgery, New York, NY, 4Brigham and Women's Hospital and Harvard Medical School, Boston, MA, 5Harvard TH Chan School of Public Health, Boston, MA, 6Brigham and Women's Hospital, Boston, MA, 7Harvard TH Chan School of Public Health, Brigham and Women's Hospital, Boston, MA
Background/Purpose: Antioxidants and vitamins present in unprocessed foods may protect against development of systemic lupus erythematosus (SLE) whereas ultra-processed foods (UPFs) remove these nutrients, adding stabilizers and emulsifiers, and may thus increase SLE risk. We assessed the association of UPF intake and SLE incidence in two cohorts of women with more than 20 years of follow-up.
Methods: We included 78,911 women in the Nurses' Health Study (NHS) followed from 1984 to 2010 and 91,079 women in NHS II followed 1991 to 2015. Diet was assessed using a validated semi-quantitative food frequency questionnaire and the NOVA food classification system was used to categorize food intake and quantity into UPF. UPFs are ready-to-eat industrial formulations that normally contain added flavors, and cosmetic additives (e.g. sugar-sweetened beverages, muffins, bagels, candies, salad dressing, and processed meat). Participants who reported new doctor-diagnosed connective tissue disease (CTD) including SLE on one of the two-year medical assessment follow-ups completed the Connective Tissue Disease Questionnaire and cases were confirmed on medical record review. Time-varying Cox regression models were used to estimate the hazard ratios (HR) and 95% confidence intervals (CI) for incident SLE. UPF intake, assessed as number of servings/day in tertiles, was the exposure. Models were adjusted for age, race, cohort, total energy intake, household income, smoking, body mass index (BMI in kg/m2), physical activity, age at menarche, oral contraceptive, multivitamin, and menopausal hormone status. We investigated effect modification by BMI in stratified models.
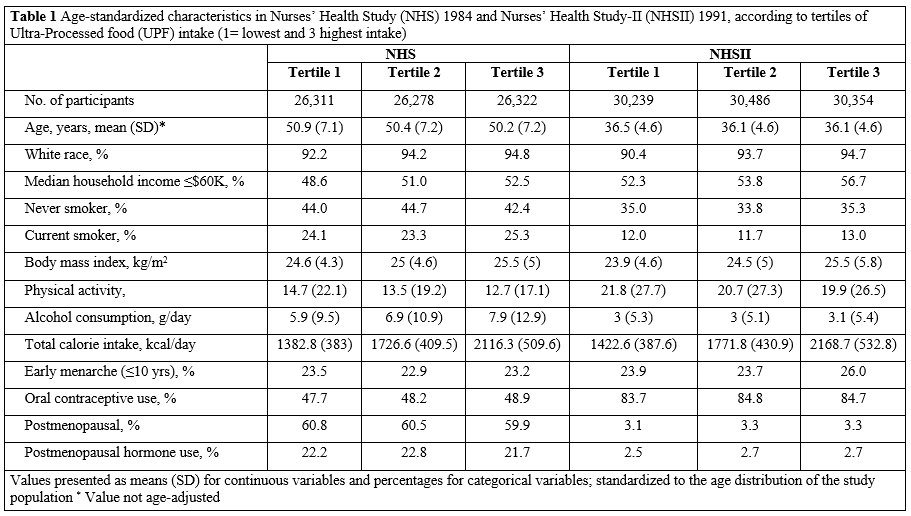
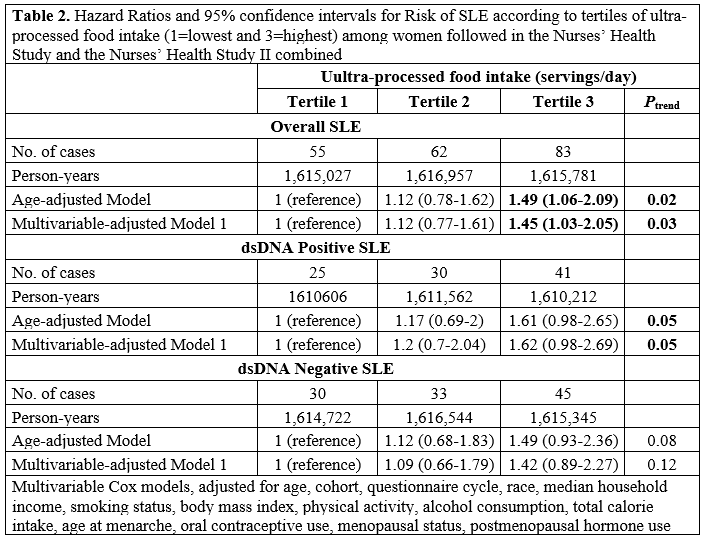
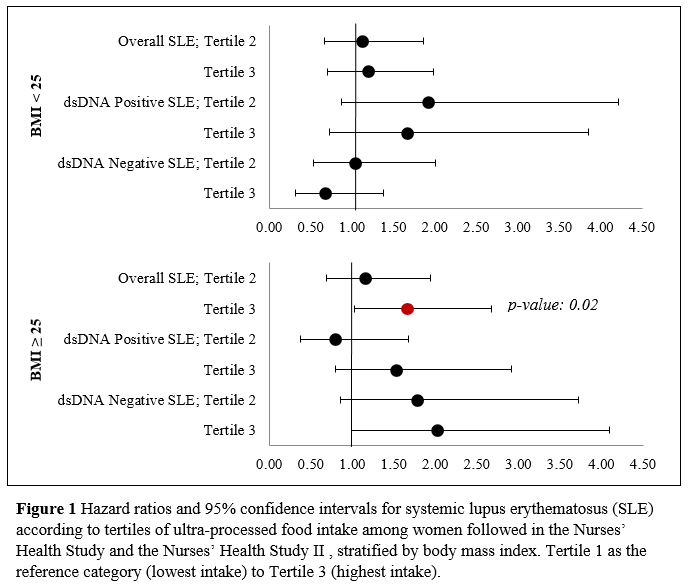
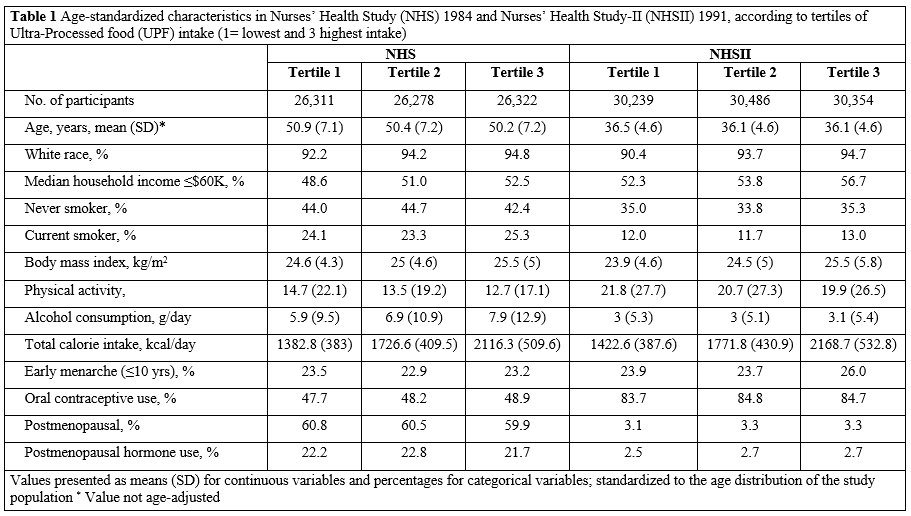
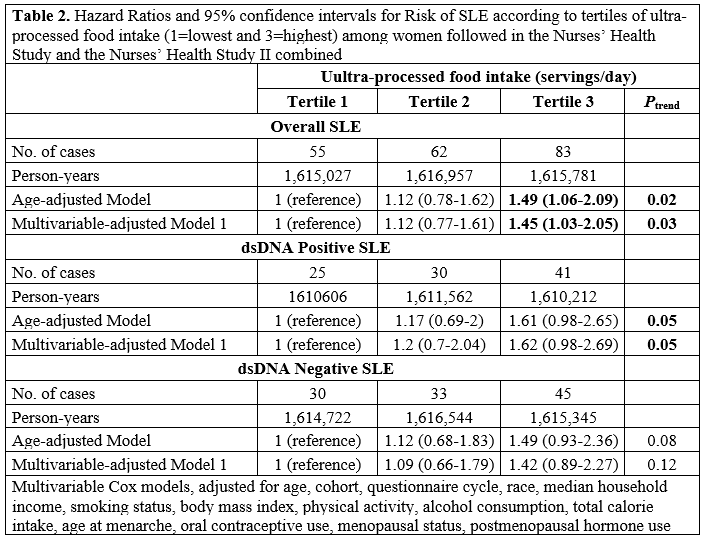
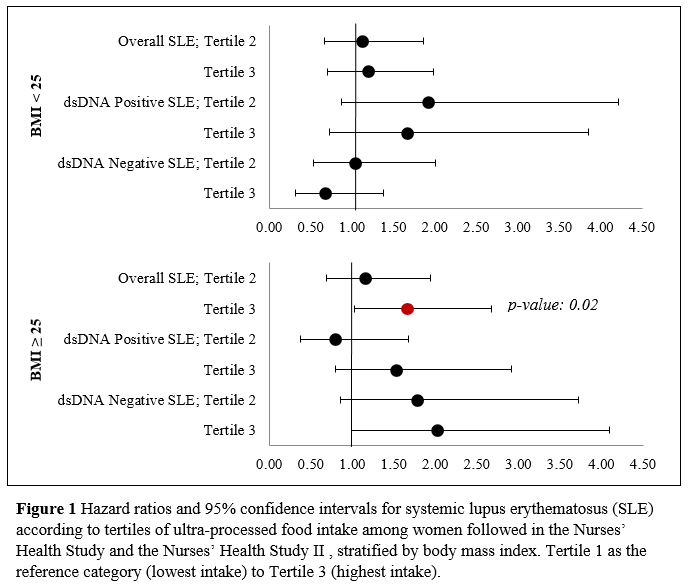
Results: Mean age at baseline was ~50 years old in NHS and ~36 years old in NHSII. (Table 1) Participants were predominantly White (90-95%). In the pooled analysis of NHS and NHSII, 200 cases of SLE were identified over 26 years follow-up in NHS and 24 years in NHSII. After multivariable adjustment, risk was higher in the 3rd than 1st UPF intake tertile (HR 1.45, 95%CI 1.03 - 2.05, p 0.03). For positive dsDNA SLE risk, the risk was also higher 1st vs. 3rd tertile (HR 1.62, 95%CI 0.98 - 2.69, p 0.05) (Table 2). Participants with BMI ≥ 25 kg/m² had higher SLE risk in the 3rd vs. 1st tertile of UPF intake servings/day (HR 1.66, 95% CI 1.03 -2.67, p 0.02) than among those with lower BMI (Figure 1).
Conclusion: Women in the highest tertile of cumulatively updated dietary UPF intake/day were at almost 50% greater risk of developing SLE compared to women in the lowest tertile of UPF daily intake. In addition, elevated SLE risk associated with high UPF intake was more significant among participants with overweight and obesity than among those with normal BMI. These novel findings deserve further study.
Disclosures: S. Rossato, None; C. Lo, None; M. Barbhaiya, None; J. Sparks, Bristol Myers Squibb, AbbVie/Abbott, Amgen, Boehringer Ingelheim, Gilead, Inova Diagnostics, Janssen, Optum, Pfizer; N. Khandpur, None; S. Malspeis, None; K. Yoshida, None; W. Willett, None; K. Costenbader, Eli Lilly, Janssen, Amgen, AstraZeneca Pharmaceuticals LP, GlaxoSmithKline(GSK), Gilead, Exagen, Neutrolis, Cel-Sci, Alkermes.
Background/Purpose: Antioxidants and vitamins present in unprocessed foods may protect against development of systemic lupus erythematosus (SLE) whereas ultra-processed foods (UPFs) remove these nutrients, adding stabilizers and emulsifiers, and may thus increase SLE risk. We assessed the association of UPF intake and SLE incidence in two cohorts of women with more than 20 years of follow-up.
Methods: We included 78,911 women in the Nurses' Health Study (NHS) followed from 1984 to 2010 and 91,079 women in NHS II followed 1991 to 2015. Diet was assessed using a validated semi-quantitative food frequency questionnaire and the NOVA food classification system was used to categorize food intake and quantity into UPF. UPFs are ready-to-eat industrial formulations that normally contain added flavors, and cosmetic additives (e.g. sugar-sweetened beverages, muffins, bagels, candies, salad dressing, and processed meat). Participants who reported new doctor-diagnosed connective tissue disease (CTD) including SLE on one of the two-year medical assessment follow-ups completed the Connective Tissue Disease Questionnaire and cases were confirmed on medical record review. Time-varying Cox regression models were used to estimate the hazard ratios (HR) and 95% confidence intervals (CI) for incident SLE. UPF intake, assessed as number of servings/day in tertiles, was the exposure. Models were adjusted for age, race, cohort, total energy intake, household income, smoking, body mass index (BMI in kg/m2), physical activity, age at menarche, oral contraceptive, multivitamin, and menopausal hormone status. We investigated effect modification by BMI in stratified models.
Results: Mean age at baseline was ~50 years old in NHS and ~36 years old in NHSII. (Table 1) Participants were predominantly White (90-95%). In the pooled analysis of NHS and NHSII, 200 cases of SLE were identified over 26 years follow-up in NHS and 24 years in NHSII. After multivariable adjustment, risk was higher in the 3rd than 1st UPF intake tertile (HR 1.45, 95%CI 1.03 - 2.05, p 0.03). For positive dsDNA SLE risk, the risk was also higher 1st vs. 3rd tertile (HR 1.62, 95%CI 0.98 - 2.69, p 0.05) (Table 2). Participants with BMI ≥ 25 kg/m² had higher SLE risk in the 3rd vs. 1st tertile of UPF intake servings/day (HR 1.66, 95% CI 1.03 -2.67, p 0.02) than among those with lower BMI (Figure 1).
Conclusion: Women in the highest tertile of cumulatively updated dietary UPF intake/day were at almost 50% greater risk of developing SLE compared to women in the lowest tertile of UPF daily intake. In addition, elevated SLE risk associated with high UPF intake was more significant among participants with overweight and obesity than among those with normal BMI. These novel findings deserve further study.
Disclosures: S. Rossato, None; C. Lo, None; M. Barbhaiya, None; J. Sparks, Bristol Myers Squibb, AbbVie/Abbott, Amgen, Boehringer Ingelheim, Gilead, Inova Diagnostics, Janssen, Optum, Pfizer; N. Khandpur, None; S. Malspeis, None; K. Yoshida, None; W. Willett, None; K. Costenbader, Eli Lilly, Janssen, Amgen, AstraZeneca Pharmaceuticals LP, GlaxoSmithKline(GSK), Gilead, Exagen, Neutrolis, Cel-Sci, Alkermes.

