Category: HIV: Epidemiology and Screening
Poster Session: HIV: Epidemiology and Screening
962 - Linkage to Care Outcomes among Known HIV-Positive Patients at a High Prevalence Urban Hospital Emergency Department

Alexander W. Sudyn
Medical Student
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Jeffrey M. Paer
Medical Student (MS4)
Rutgers New Jersey Medical School, Newark, NJ
Bloomfield, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.

Swetha Kodali
Medical Student
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SM
Samuel Maldonado
Resident Physician
University of Virginia
Charlottesville, VirginiaDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- AN
Amesika Nyaku
Assistant Professor
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
- SS
Shobha Swaminathan
Associate Professor
Rutgers New Jersey Medical School
Newark, New JerseyDisclosure: I do not have any relevant financial / non-financial relationships with any proprietary interests.
Presenting Author(s)
Co-Author(s)
Background:
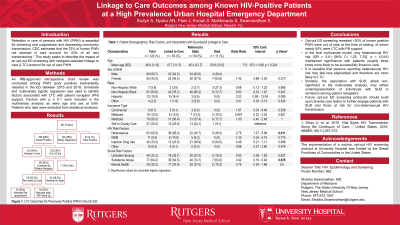
Retention in care of persons with HIV (PWH) is essential for achieving viral suppression and decreasing community transmission. CDC estimates that the 23% of known PWH not retained in care account for 43% of all new transmissions. This study seeks to describe the impact of an opt-out ED screening with navigator-assisted linkage to care (LTC) protocol for out of care PWH.
Methods:
An IRB-approved retrospective chart review was conducted among PWH (prior positive) inadvertently retested in the ED between 2015 and 2018. Univariate and multivariate logistic regression was used to identify factors associated with LTC with patient navigator (PN) support. Factors with p ≤ 0.1 were included in the multivariate analysis as were age and sex at birth. Patients who died were excluded from statistical analyses.
Results:
Among 464 patients who tested positive, 338 (73%) were known positive with 120 (35%) of those out of care at the time of screening. Mean age for this group was 47 (SD 11.9); 57% male, 81% non-Hispanic black, 10% Hispanic, and 6% non-Hispanic white. Fifty-five (46%) patients were successfully LTC, 54 (45%) referred to the state for linkage, and 11 (9%) died. A total of 109 patients were included in the analysis. Univariate analysis was performed for age (F(1, 107) = 0.98, p = 0.324) and female sex at birth (OR = 1.42 [95% CI 0.66, 3.05], p = 0.373) as well as Hispanic race (OR = 3.33 [95% CI 0.84, 13.04], p = 0.085), heterosexual HIV risk (OR = 2.76 [95% CI 1.27, 5.99], p = 0.011), IDU (OR = 0.49 [95% CI 0.21, 1.11], p = 0.088), and other SUD (OR = 0.42 [95% CI 0.19, 0.94], p = 0.035). Only heterosexual HIV risk (OR = 3.01 [95% CI 1.23, 7.32], p = 0.015) maintained significance in the final multivariate model.
Conclusion: Opt-out ED screening revealed >30% of known positive PWH were out of care at the time of testing; of whom nearly 50% were LTC with PN support. It is possible that persons reporting heterosexual HIV risk may feel less stigmatized and therefore are more likely to LTC. Similarly, the association with SUD, albeit non-significant, may reflect underrepresentation of individuals with SUD in remission among patient navigators. Future opt-out ED screening protocols should build upon diverse care teams to further engage patients with SUD and those at risk for non-heterosexual HIV transmission.

