Nonvascular Interventions
Safety and Efficacy of Percutaneous Management of Acute Cholangitis

Asad Malik, MD
Clinical Research Fellow
Northwestern UniversityDisclosure(s): No financial relationships to disclose
- Is
Isabella strolia, n/a
PA Student
Northwestern University - YM
Yasaman Moazeni, MD
Research Fellow
Northwestern University - MP
Muhammed Ebrahim Patel, MD
Research Fellow
Northwestern University 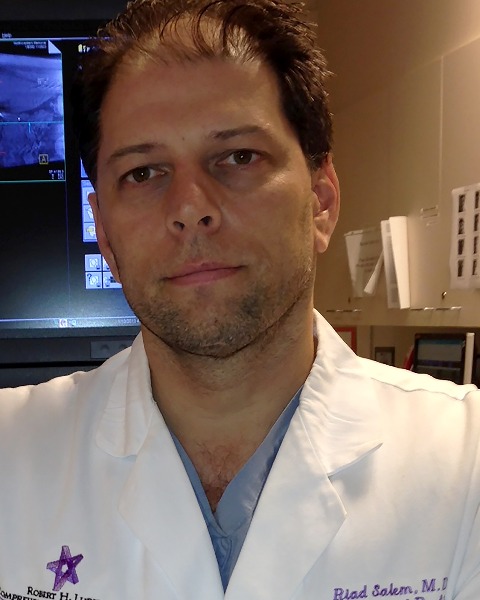
Riad Salem, MD
Chief of Vascular and Interventional Radiology in the Department of Radiology
Northwestern Memorial Hospital
Ahsun Riaz, MD
Interventional Radiologist
Northwestern University
Poster Presenter(s)
Author/Co-author(s)
Acute cholangitis can lead to severe complications if poorly managed. Peroral endoscopic biliary drainage is not feasible in some patients, such as those with altered biliary anatomy. Interventional radiology (IR) can play a significant role by performing transhepatic/transjejunal biliary drainage in these patients. This study aims to describe interventions performed in patients with acute cholangitis and to study the impact of these interventions.
Materials and Methods:
Percutaneous transhepatic/transjejunal interventions were performed in 449 consecutive patients between 2009-2021. Of these, 69 (15%) patients (73 cases) had acute cholangitis before the intervention. The mean age was 61.8 (range: 18-94), 36 patients were males, 31 had benign etiologies (38 malignant), 30 had prior hepatobiliary surgeries, 35 had prior ERCPs, and 27 patients had prior biliary stents. Tokyo guidelines were used to grade acute cholangitis. Paired samples Wilcoxon test was utilized to compare pre- and 1-2 months post-white blood cell (WBC) count, total bilirubin, and alkaline phosphatase (ALP).
Results:
Twenty-four (33%) cases had grade 1 cholangitis, 18 (25%) had grade 2 and 31 (42%) had grade 3 cholangitis according to the Tokyo guidelines. The average time from presentation to first IR intervention was 3.96 days (range 0-13 days). Biliary drains were placed in 70 (96%) cases, cholangioplasty was performed in 14 (19%), and stents were placed in 4 (5%) cases in the first session. The median decrease in pre- and post-intervention WBC count, total bilirubin, and ALP was 2.9 x 109/L, 1.7 mg/dL and 155 IU/L, respectively (P=0.14, 0.006 and 0.001, respectively). The average duration of hospital stay after IR intervention was 9.13 days (range: 0-69 days), and 21 (29%) cases were admitted to ICU. In 31 (42%) cases, acute cholangitis had progressed to sepsis before the IR intervention. In 23/31 (74%) cases, sepsis was resolved within a week of IR intervention, whereas in 8/31 (26%) cases, sepsis was resolved within two weeks of IR intervention. Major complication was seen in one (1%) case (bleeding, managed by embolization) and minor complications (e.g., pericatheter leak/occlusion, malpositioned drain) were seen in 22 (30%) cases.
Conclusion:
IR plays an essential role in managing acute cholangitis, which needs urgent diagnosis and treatment. Percutaneous drainage is safe and effective in the management of acute cholangitis.

.jpg)
.jpg)
.png)
.png)
.png)
.png)
.jpg)
.png)
.png)