Back
Women’s Health
074 - Why So Vascular? Endovascular Management of a Complex Vascular Lesion in an Obstetric Patient
Nicholas Voutsinas, MD – Assistant Professor of Radiology and Radiologic Sciences, Radiology, Vanderbilt University Medical Center
Purpose: Uterine vascular lesions are a life-threatening cause of vaginal bleeding in obstetric patients. They present a diagnostic challenge due to overlapping features and occasional co-existence. This case discusses a 35-year-old female with vaginal bleeding following a medical abortion, later found to have retained products of conception (RPOC). Uterine artery embolization (UAE), performed earlier in her course, had revealed a coexisting pseudoaneurysm. The UAE aided in diagnosis and allowed for safe subsequent dilation and curettage/evacuation (D&C/E) of the RPOC.
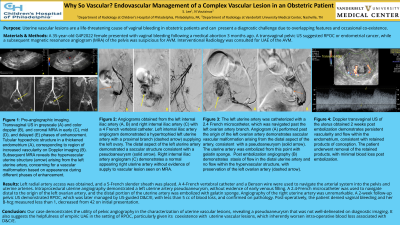
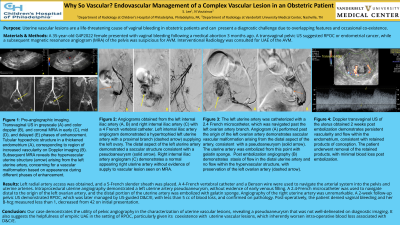
Material and Methods: A 35-year-old G4P2022 female presented with vaginal bleeding following a medical abortion 3 months ago. Three days prior to presentation, the patient was seen at an outside hospital where a pelvic ultrasound (US) suggested arteriovenous malformation (AVM). The patient was transfused for anemia and discharged. On current admission to the hospital, a transvaginal pelvic US suggested RPOC or endometrial cancer, while a subsequent magnetic resonance (MR) of the pelvis was suspicious for AVM. Interventional Radiology was consulted for UAE of the AVM.
Results: Left radial artery access was obtained, and a 5-French slender sheath was placed. A 4-French vertebral catheter and a Benson wire were used to navigate the arterial system into the pelvis and uterine arteries. Intraprocedural uterine angiography demonstrated a left uterine artery pseudoaneurysm, without evidence of early venous filling. A 2.4-French microcatheter was used to navigate distal to the origin of the left ovarian artery, and the distal portion of the uterine artery was embolized with gelatin sponge. Angiography of the right uterine artery was unremarkable. A 2-week follow-up pelvic US demonstrated RPOC, which was later managed by US-guided D&C/E, with less than 5 cc of blood loss, and confirmed on pathology. Post-operatively, the patient denied vaginal bleeding and her B-hcg measured less than 1, decreased from 42 on initial presentation.
Conclusions: Our case demonstrates the utility of pelvic angiography in the characterization of uterine vascular lesions, revealing a pseudoaneurysm that was not well-delineated on non-invasive diagnostic imaging. It also suggests the helpfulness of empiric UAE in the setting of RPOC, particularly given potential coexistence of uterine vascular lesions, which can inherently worsen intra-operative blood loss associated with D&C/E.
Material and Methods: A 35-year-old G4P2022 female presented with vaginal bleeding following a medical abortion 3 months ago. Three days prior to presentation, the patient was seen at an outside hospital where a pelvic ultrasound (US) suggested arteriovenous malformation (AVM). The patient was transfused for anemia and discharged. On current admission to the hospital, a transvaginal pelvic US suggested RPOC or endometrial cancer, while a subsequent magnetic resonance (MR) of the pelvis was suspicious for AVM. Interventional Radiology was consulted for UAE of the AVM.
Results: Left radial artery access was obtained, and a 5-French slender sheath was placed. A 4-French vertebral catheter and a Benson wire were used to navigate the arterial system into the pelvis and uterine arteries. Intraprocedural uterine angiography demonstrated a left uterine artery pseudoaneurysm, without evidence of early venous filling. A 2.4-French microcatheter was used to navigate distal to the origin of the left ovarian artery, and the distal portion of the uterine artery was embolized with gelatin sponge. Angiography of the right uterine artery was unremarkable. A 2-week follow-up pelvic US demonstrated RPOC, which was later managed by US-guided D&C/E, with less than 5 cc of blood loss, and confirmed on pathology. Post-operatively, the patient denied vaginal bleeding and her B-hcg measured less than 1, decreased from 42 on initial presentation.
Conclusions: Our case demonstrates the utility of pelvic angiography in the characterization of uterine vascular lesions, revealing a pseudoaneurysm that was not well-delineated on non-invasive diagnostic imaging. It also suggests the helpfulness of empiric UAE in the setting of RPOC, particularly given potential coexistence of uterine vascular lesions, which can inherently worsen intra-operative blood loss associated with D&C/E.
