Back
Women’s Health
085 - Urgent Pelvic Venous Insufficiency Treatment in Lieu of Hysterectomy for Blood Loss Anemia in Pregnancy
Sean Duguay, M.D. – Associate Professor, Interventional Radiology, University of Oklahoma Health Sciences Center
Purpose: To present a unique case of pelvic venous insufficiency (PVI) for which embolization was both successful and life-saving for persistent cervical varicose vein hemorrhage in the setting of pregnancy.
Material and Methods: 41-year-old female presented to labor and delivery at 15 weeks gestation for recurrent vaginal bleeding and acute blood loss anemia. Conservative treatment with blood transfusions and RhoGam had recently failed. On admission, a transvaginal ultrasound performed by maternal fetal medicine raised concern for abnormal cervical tissue vascularity and possible uterine or cervical arteriovenous malformation (AVM). Interventional radiology (IR) was consulted for emergent arterial embolization, for which the alternative was emergent hysterectomy. Pelvic arteriography was negative for AVM or other acute arterial injury. Repeat ultrasound, with IR present at bedside, demonstrated slow flow vessels in the cervix representing cervical varices. With hysterectomy imminent, the patient was brought back to the interventional suite and pelvic venography performed.
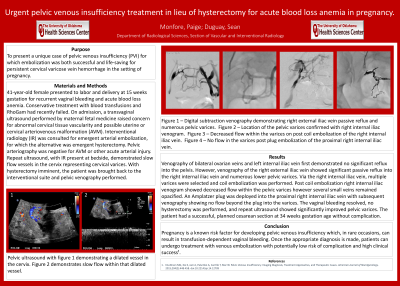
Results: Venography of bilateral ovarian veins and left internal iliac vein first demonstrated no significant reflux into the pelvis. However, venography of the right femoral vein showed significant passive reflux into the right internal iliac vein and numerous lower pelvic varices. Via the right internal iliac vein, multiple varices were selected and coil embolization was performed. Post coil embolization right internal iliac venogram showed decreased flow within the pelvic varices however several small veins remained opacified. An Amplatzer plug was deployed into the proximal right internal iliac vein with subsequent venography showing no flow beyond the plug into the varices. The vaginal bleeding resolved, no hysterectomy was performed, and repeat ultrasound showed significantly improved pelvic varices. The patient had a successful, planned cesarean section at 34 weeks gestation age without complication.
Conclusions: Pregnancy is a known risk factor for developing pelvic venous insufficiency, which in rare occasions, can result in transfusion-depending vaginal bleeding. Once the appropriate diagnosis is made, patients can undergo treatment with venous embolization with potentially low risk of complication and high clinical success.
Material and Methods: 41-year-old female presented to labor and delivery at 15 weeks gestation for recurrent vaginal bleeding and acute blood loss anemia. Conservative treatment with blood transfusions and RhoGam had recently failed. On admission, a transvaginal ultrasound performed by maternal fetal medicine raised concern for abnormal cervical tissue vascularity and possible uterine or cervical arteriovenous malformation (AVM). Interventional radiology (IR) was consulted for emergent arterial embolization, for which the alternative was emergent hysterectomy. Pelvic arteriography was negative for AVM or other acute arterial injury. Repeat ultrasound, with IR present at bedside, demonstrated slow flow vessels in the cervix representing cervical varices. With hysterectomy imminent, the patient was brought back to the interventional suite and pelvic venography performed.
Results: Venography of bilateral ovarian veins and left internal iliac vein first demonstrated no significant reflux into the pelvis. However, venography of the right femoral vein showed significant passive reflux into the right internal iliac vein and numerous lower pelvic varices. Via the right internal iliac vein, multiple varices were selected and coil embolization was performed. Post coil embolization right internal iliac venogram showed decreased flow within the pelvic varices however several small veins remained opacified. An Amplatzer plug was deployed into the proximal right internal iliac vein with subsequent venography showing no flow beyond the plug into the varices. The vaginal bleeding resolved, no hysterectomy was performed, and repeat ultrasound showed significantly improved pelvic varices. The patient had a successful, planned cesarean section at 34 weeks gestation age without complication.
Conclusions: Pregnancy is a known risk factor for developing pelvic venous insufficiency, which in rare occasions, can result in transfusion-depending vaginal bleeding. Once the appropriate diagnosis is made, patients can undergo treatment with venous embolization with potentially low risk of complication and high clinical success.
