Back

Session: Oral Abstract Session
CSI04 - Comparison of the Effects of Pharmacotherapy Versus Action Potential Simulation Therapy in Patients with Mild to Moderate Temporomandibular Disorders: A Randomized Clinical Trial
Saturday, March 11, 2023
4:15pm – 4:25pm CST
Table 1: Data pertinent to joint pain

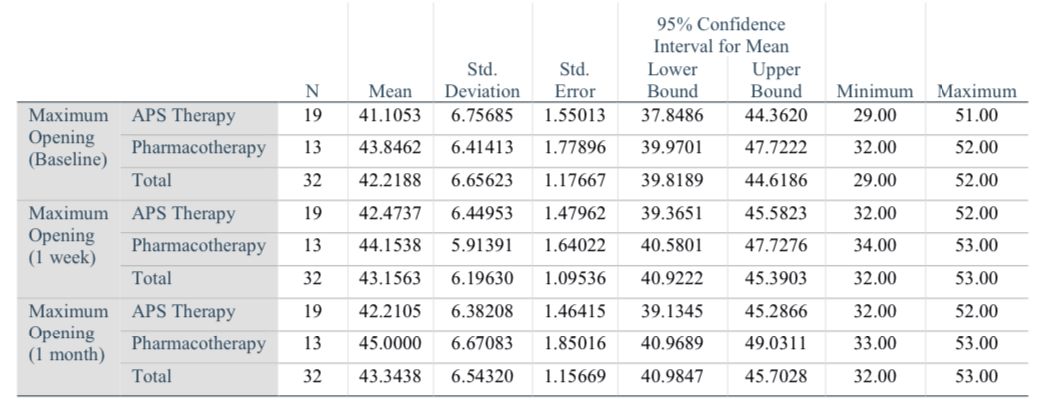
Table 2: Data pertinent to mandibular maximum opening
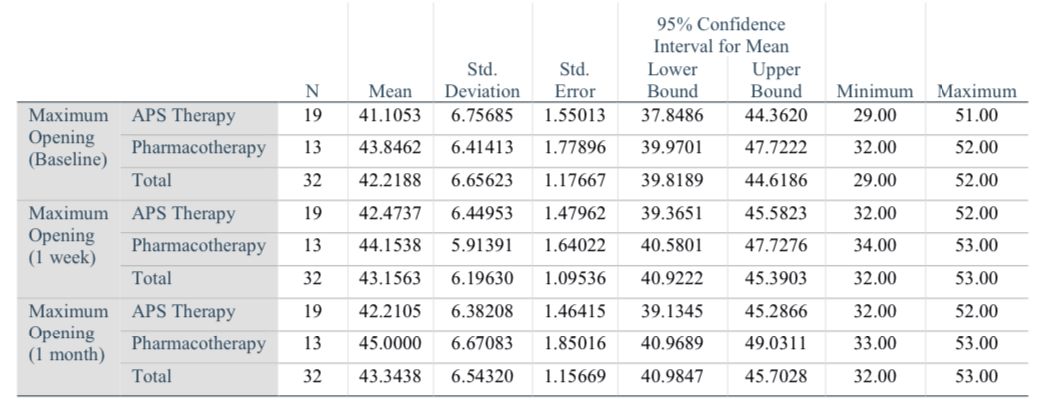
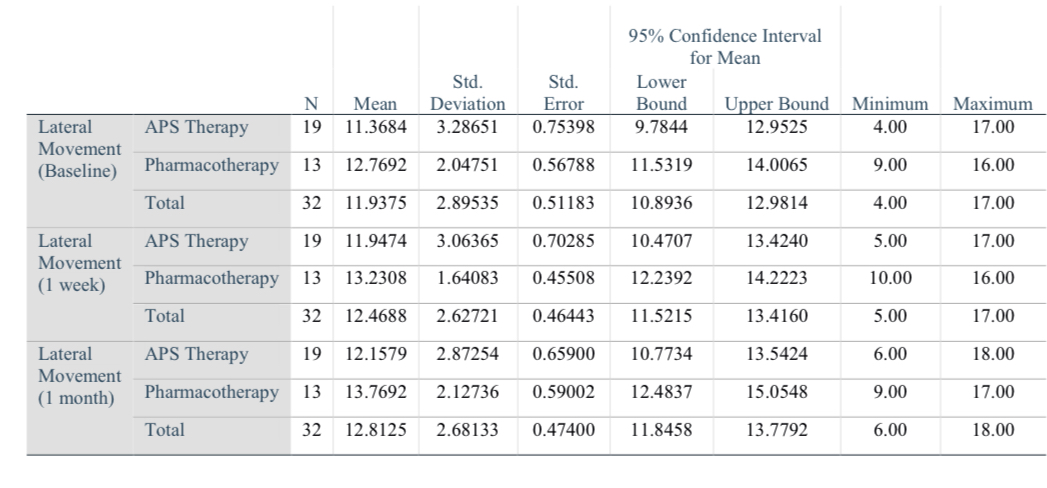
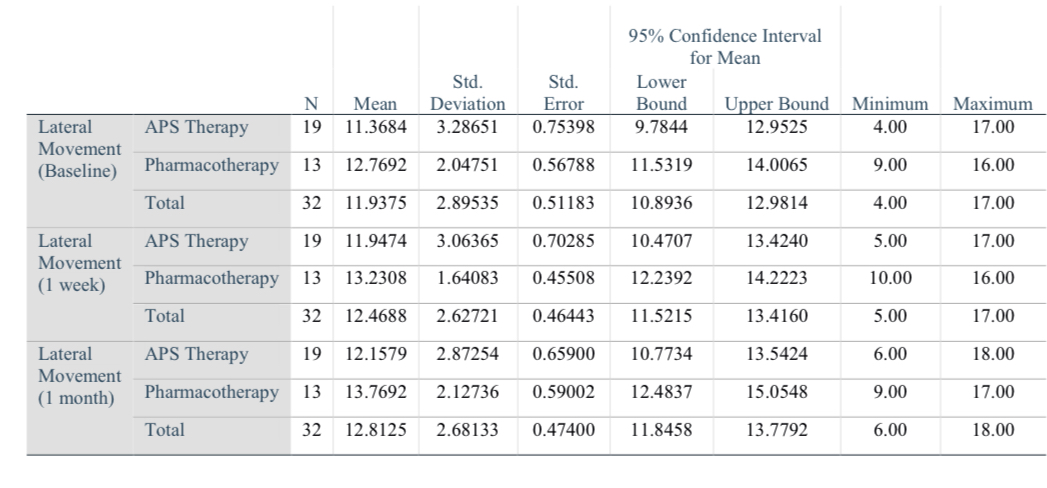
Table 3: Data pertinent to mandibular lateral movement
.jpg)
Ramtin Dastgir, DDS
Research Fellow
Department of Oral and Maxillofacial Surgery, Case Western Reserve University
Cleveland, OhioDisclosure(s): No financial relationships to disclose
Oral Abstract Presenter(s)
Abstract: Temporomandibular disorders (TMDs) are the second most prevalent etiology of orofacial pains following odontogenic causes, which have been recorded in recent studies to account for up to 41% of the general population. These disorders can significantly affect one’s quality of life by altering their sleep patterns, inducing stress and anxiety, and causing depression in some cases. To date, the main pathophysiology of this disorder has remained unclear; however, some studies have demonstrated the etiology of TMDs to be multi-factorial. Preliminary treatments of TMDs are non-invasive and include but are not limited to: physiotherapy, pharmacotherapy, electrotherapy, laser therapy, and splint therapy. Action Potential Simulation (APS) therapy is a relatively novel approach based on simulation and induction of physiological neural impulses down specific neural pathways and therefore imitation of physiological action potentials. Researches have demonstrated its capability in reduction of pain, inflammation, edema, increasing local circulation, and cell regeneration.
This prospective randomized clinical trial aimed to compare and asses the effects of APS therapy with pharmacotherapy approaches. 32 patients with chronic, mild to moderate TMDs according to DC-TMD guidelines were selected and were randomly allocated into two groups. One group received APS therapy and one received pharmacotherapy based on the common three-drug regimen of NSAID (Naproxen), muscle relaxants (Cyclobenzaprine), and benzodiazepine (Diazepam). Temporomandibular joint pain, sounds, maximum mandibular lateral movement, and maximum opening were assessed in this study.
The obtained results demonstrated that there are no statistically significant (P>0.05) differences in terms of temporomandibular joint pain, sounds, maximum mandibular lateral movement, and maximum opening between the two groups in one-week and one-month follow-ups and APS therapy had achieved similar results with significantly less side effects and fewer treatment duration.
It can be concluded that APS therapy can be safely and effectively utilized as an independent approach or it can be used as an adjunctive therapy along with other treatment modalities in treatment of chronic mild to moderate TMDs.
1. Małgorzata P, Małgorzata K-M, Karolina C, Gala A. Diagnostic of temporomandibular disorders and other facial pain conditions-narrative review and personal experience. Medicina (Kaunas). 2020;56(9):472.
2. Pyszora A, Krajnik M, Graczyk M, Adamczyk A, Budzyński J, Lukowicz M, et al. 828 analgesic efficacy of aps (action potential simulation). Pilot study at the patients with chronic pain in musculoskeletal disorders. Eur J Pain. 2006;10(S1):S215b–215.
This prospective randomized clinical trial aimed to compare and asses the effects of APS therapy with pharmacotherapy approaches. 32 patients with chronic, mild to moderate TMDs according to DC-TMD guidelines were selected and were randomly allocated into two groups. One group received APS therapy and one received pharmacotherapy based on the common three-drug regimen of NSAID (Naproxen), muscle relaxants (Cyclobenzaprine), and benzodiazepine (Diazepam). Temporomandibular joint pain, sounds, maximum mandibular lateral movement, and maximum opening were assessed in this study.
The obtained results demonstrated that there are no statistically significant (P>0.05) differences in terms of temporomandibular joint pain, sounds, maximum mandibular lateral movement, and maximum opening between the two groups in one-week and one-month follow-ups and APS therapy had achieved similar results with significantly less side effects and fewer treatment duration.
It can be concluded that APS therapy can be safely and effectively utilized as an independent approach or it can be used as an adjunctive therapy along with other treatment modalities in treatment of chronic mild to moderate TMDs.
1. Małgorzata P, Małgorzata K-M, Karolina C, Gala A. Diagnostic of temporomandibular disorders and other facial pain conditions-narrative review and personal experience. Medicina (Kaunas). 2020;56(9):472.
2. Pyszora A, Krajnik M, Graczyk M, Adamczyk A, Budzyński J, Lukowicz M, et al. 828 analgesic efficacy of aps (action potential simulation). Pilot study at the patients with chronic pain in musculoskeletal disorders. Eur J Pain. 2006;10(S1):S215b–215.
