Back
Introduction: The evaluation and treatment of female sexual dysfunction (FSD) has been slow to progress. In 2004, the American Urogynecology Society (AUGS) surveyed its members to assess practice patterns for FSD. The objective of this study was to administer a similar survey to current members of AUGS and the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) to evaluate existing practice patterns.
Methods: An electronic survey based on a prior survey administered to AUGS members in 2004 was distributed to current SUFU and AUGS members. The results were compared.
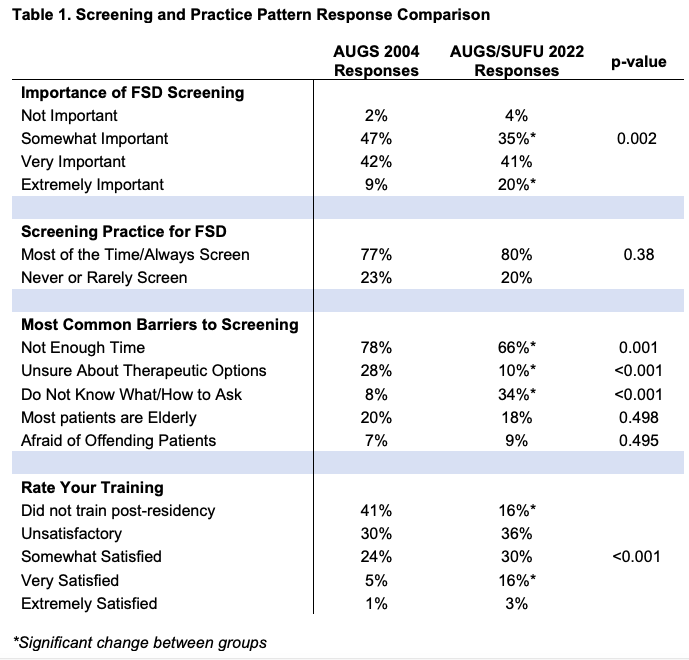
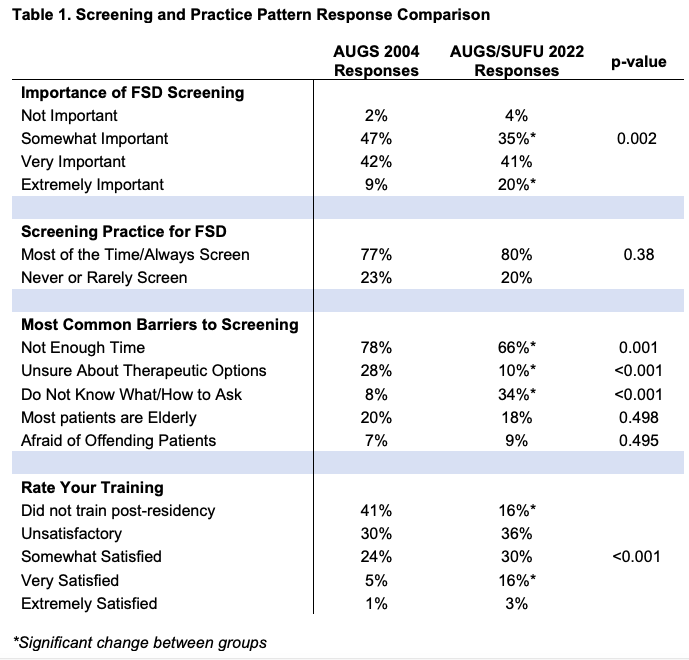
Results: 187 physicians responded. The majority were female (75%). Respondent experience was <5 years in practice (25%), 5-10 years (20%), 11-20 years (17%), >20 years (22%), or currently in fellowship (16%). Fifty-four percent were at an academic or university-based practice. Physicians assessed FSD by asking about sexual activity (89%), dyspareunia (89%), arousal (33%), libido (29%), and orgasm (21%), while few reported using validated questionnaires (19%). Most physicians (54%) responded they perceived the overall incidence of FSD ranged 21-50%. Screening practices and barriers are listed in Table 1 and compared to the responses from AUGS members in 2004. The majority of current responders had post-residency training (84% vs. 59% in 2004, p<0.001). 20% of current members consider FSD screening to be extremely important versus 9% in 2004 (p = 0.002). Most common reason for not screening was time constraints. Current practitioners also report not screening because they do not know how/what to ask, whereas in 2004 physicians were more unsure about therapeutic options (p <0.001). In regards to post residency training, 52% were less than satisfied, significantly improved compared to 71% in 2004 (p <0.001). Eighty-seven percent of current AUGS/SUFU members would feel comfortable referring patients to an interactive phone application about FSD.
Conclusions: Screening patterns and barriers to treatment of FSD have remained relatively unchanged over the last 18 years, with the most common barrier being time constraints. Many FPMRS/urogynecology trainees continue to feel unsatisfied with FSD training. In the future, phone applications may be a good resource when practitioners are uncomfortable or have a lack of time to discuss FSD. SOURCE OF
Funding: None
Podium Session
Session: PD26: Sexual Function/Dysfunction: Evaluation II
PD26-05: Female Sexual Dysfunction: Practice Patterns & Patient Education Among SUFU and AUGS Members
Sunday, April 30, 2023
7:40 AM – 7:50 AM CST
Location: S501C
- PS
Podium Presenter(s)
Introduction: The evaluation and treatment of female sexual dysfunction (FSD) has been slow to progress. In 2004, the American Urogynecology Society (AUGS) surveyed its members to assess practice patterns for FSD. The objective of this study was to administer a similar survey to current members of AUGS and the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) to evaluate existing practice patterns.
Methods: An electronic survey based on a prior survey administered to AUGS members in 2004 was distributed to current SUFU and AUGS members. The results were compared.
Results: 187 physicians responded. The majority were female (75%). Respondent experience was <5 years in practice (25%), 5-10 years (20%), 11-20 years (17%), >20 years (22%), or currently in fellowship (16%). Fifty-four percent were at an academic or university-based practice. Physicians assessed FSD by asking about sexual activity (89%), dyspareunia (89%), arousal (33%), libido (29%), and orgasm (21%), while few reported using validated questionnaires (19%). Most physicians (54%) responded they perceived the overall incidence of FSD ranged 21-50%. Screening practices and barriers are listed in Table 1 and compared to the responses from AUGS members in 2004. The majority of current responders had post-residency training (84% vs. 59% in 2004, p<0.001). 20% of current members consider FSD screening to be extremely important versus 9% in 2004 (p = 0.002). Most common reason for not screening was time constraints. Current practitioners also report not screening because they do not know how/what to ask, whereas in 2004 physicians were more unsure about therapeutic options (p <0.001). In regards to post residency training, 52% were less than satisfied, significantly improved compared to 71% in 2004 (p <0.001). Eighty-seven percent of current AUGS/SUFU members would feel comfortable referring patients to an interactive phone application about FSD.
Conclusions: Screening patterns and barriers to treatment of FSD have remained relatively unchanged over the last 18 years, with the most common barrier being time constraints. Many FPMRS/urogynecology trainees continue to feel unsatisfied with FSD training. In the future, phone applications may be a good resource when practitioners are uncomfortable or have a lack of time to discuss FSD. SOURCE OF
Funding: None