Back
Introduction: Little data exists on the optimal timing for intervention for symptomatic kidney stones, as such, our objective was to determine the impact of early intervention versus delayed intervention/expectant management for patients presenting to the emergency department (ED) with renal colic
Methods: We conducted a population-based cohort study in the province of Ontario, utilizing linked administrative health data. Patients who presented to an ED with renal colic between April 1, 2010 to June 30, 2020 were included. Patients were divided into two groups. The early intervention (EI) group underwent shockwave lithotripsy (SWL), ureteroscopy (URS) or percutaneous nephrolithotomy (PCNL) within 2-weeks of presentation. The delayed intervention/expectant management (non-EI) group represented all other patients. Patients were followed forward in time for 3 months in the EI group and for 4 weeks post-intervention or 3 months (whichever was longer) in the non-EI group to assess for our outcomes. The outcomes included additional ED visits, hospitalizations or imaging studies, stent or nephrostomy insertion and urologist/primary care visits. These outcomes were compared across the two groups using matched propensity score modelling.
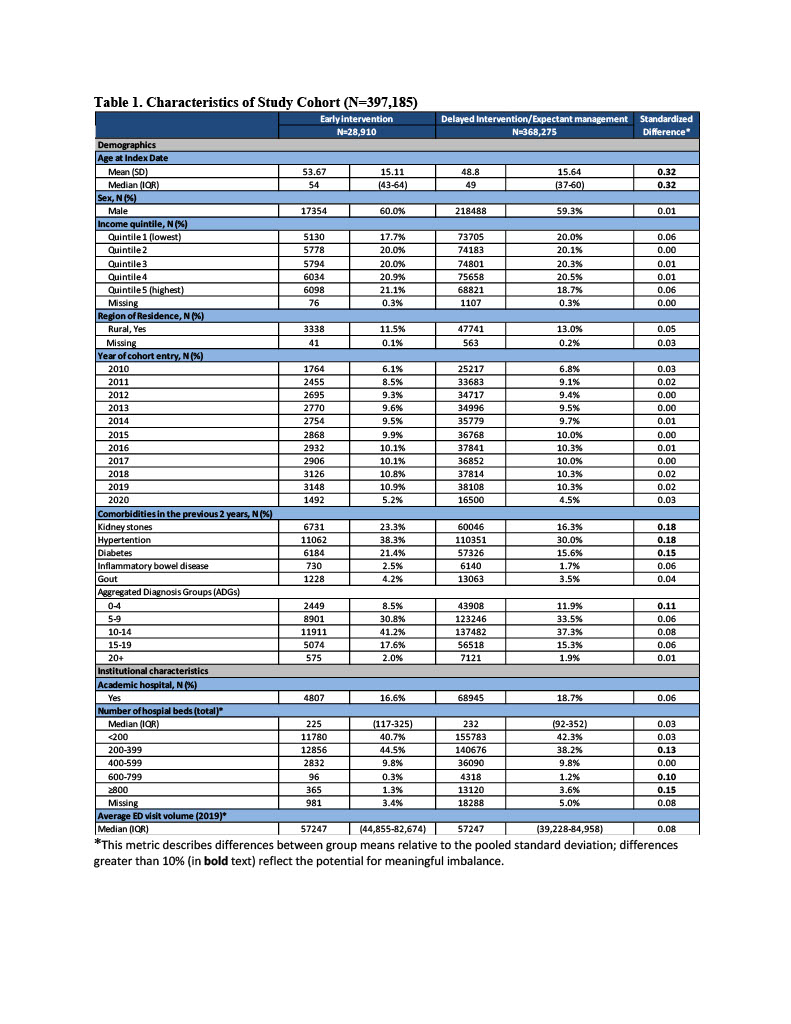
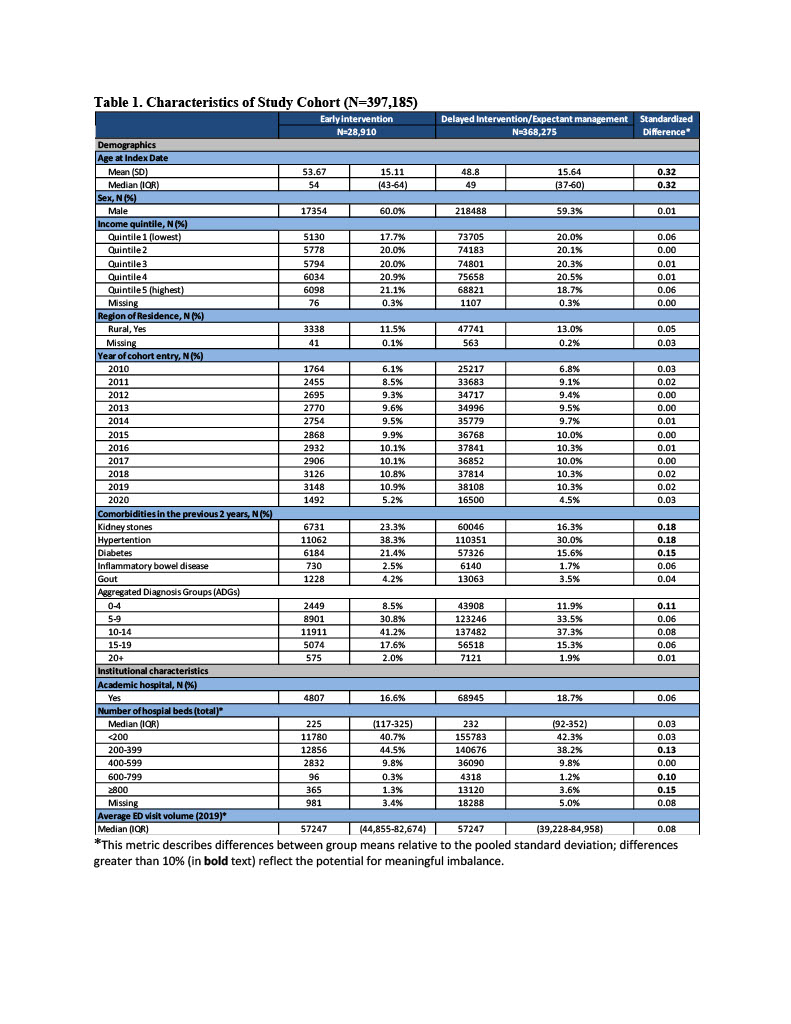
Results: There were 397,185 index renal colic events (EI=28,910, non-EI=368,275). The EI group was slightly older and more likely to have a history for stones, hypertension and diabetes (Table 1). The EI group had a lower risk for additional ED visits (RR 0.70 95% CI 0.68-0.72, p<0.001) and hospital admissions (RR 0.52, 95% CI 0.50-0.55, p<0.001) compared to the non-EI group. Similarly, the EI group had a lower risk for stent (RR 0.62, 95% CI 0.54-0.71, p<0.001) or nephrostomy insertion (RR 0.49, 95% CI 0.42-0.57, p<0.001), however there was no difference for additional imaging. The EI group had a slightly increased risk for urologist/primary care visit (RR 1.02, 95% CI 1.02-1.03, p<0.001). In the non-EI group, 17 % underwent eventual intervention.
Conclusions: Our population-based study suggests a benefit to EI for those presenting with renal colic to the ED, but potentially with the risk of exposing some patients to unneeded treatment. These findings could influence practice patterns and guideline recommendations moving forward. SOURCE OF
Funding: Northeastern Section of the AUA
Moderated Poster Session
Session: MP16: Stone Disease: Epidemiology & Evaluation I
MP16-03: The Impact of Timing of Definitive Intervention for Patients with Acute Renal Colic: A Population-Based Study
Friday, April 28, 2023
1:00 PM – 3:00 PM CST
Location: S405
- MO
Michael Ordon
MD, MSc, FRCSC
University of Toronto
Poster Presenter(s)
Introduction: Little data exists on the optimal timing for intervention for symptomatic kidney stones, as such, our objective was to determine the impact of early intervention versus delayed intervention/expectant management for patients presenting to the emergency department (ED) with renal colic
Methods: We conducted a population-based cohort study in the province of Ontario, utilizing linked administrative health data. Patients who presented to an ED with renal colic between April 1, 2010 to June 30, 2020 were included. Patients were divided into two groups. The early intervention (EI) group underwent shockwave lithotripsy (SWL), ureteroscopy (URS) or percutaneous nephrolithotomy (PCNL) within 2-weeks of presentation. The delayed intervention/expectant management (non-EI) group represented all other patients. Patients were followed forward in time for 3 months in the EI group and for 4 weeks post-intervention or 3 months (whichever was longer) in the non-EI group to assess for our outcomes. The outcomes included additional ED visits, hospitalizations or imaging studies, stent or nephrostomy insertion and urologist/primary care visits. These outcomes were compared across the two groups using matched propensity score modelling.
Results: There were 397,185 index renal colic events (EI=28,910, non-EI=368,275). The EI group was slightly older and more likely to have a history for stones, hypertension and diabetes (Table 1). The EI group had a lower risk for additional ED visits (RR 0.70 95% CI 0.68-0.72, p<0.001) and hospital admissions (RR 0.52, 95% CI 0.50-0.55, p<0.001) compared to the non-EI group. Similarly, the EI group had a lower risk for stent (RR 0.62, 95% CI 0.54-0.71, p<0.001) or nephrostomy insertion (RR 0.49, 95% CI 0.42-0.57, p<0.001), however there was no difference for additional imaging. The EI group had a slightly increased risk for urologist/primary care visit (RR 1.02, 95% CI 1.02-1.03, p<0.001). In the non-EI group, 17 % underwent eventual intervention.
Conclusions: Our population-based study suggests a benefit to EI for those presenting with renal colic to the ED, but potentially with the risk of exposing some patients to unneeded treatment. These findings could influence practice patterns and guideline recommendations moving forward. SOURCE OF
Funding: Northeastern Section of the AUA