Back
Introduction: Partial nephrectomy (PN) is a preferred option for management of small renal masses due to benefits in postoperative renal function offered by preservation of normal parenchyma when compared to radical nephrectomy (RN). PN is a technically challenging procedure, requiring a high level of expertise to achieve negative margins and minimize blood loss and ischemia times. Considering increased interest in minimally invasive surgery (MIS) and the rapid adoption of robotic surgery within the field of urology, our study aims to elucidate contemporary trends in surgical approach for PN and RN and analyze patient and facility characteristics associated with treatment choice.
Methods: We used the National Inpatient Sample to identify patients diagnosed with malignant neoplasm of the kidney treated with PN or RN from 2014 to 2019. We examined trends in surgical approach (open, laparoscopic, and robotic) over the study period using a Wilcoxon-type test for trend and performed multivariable logistic regression modeling to determine relevant covariates.
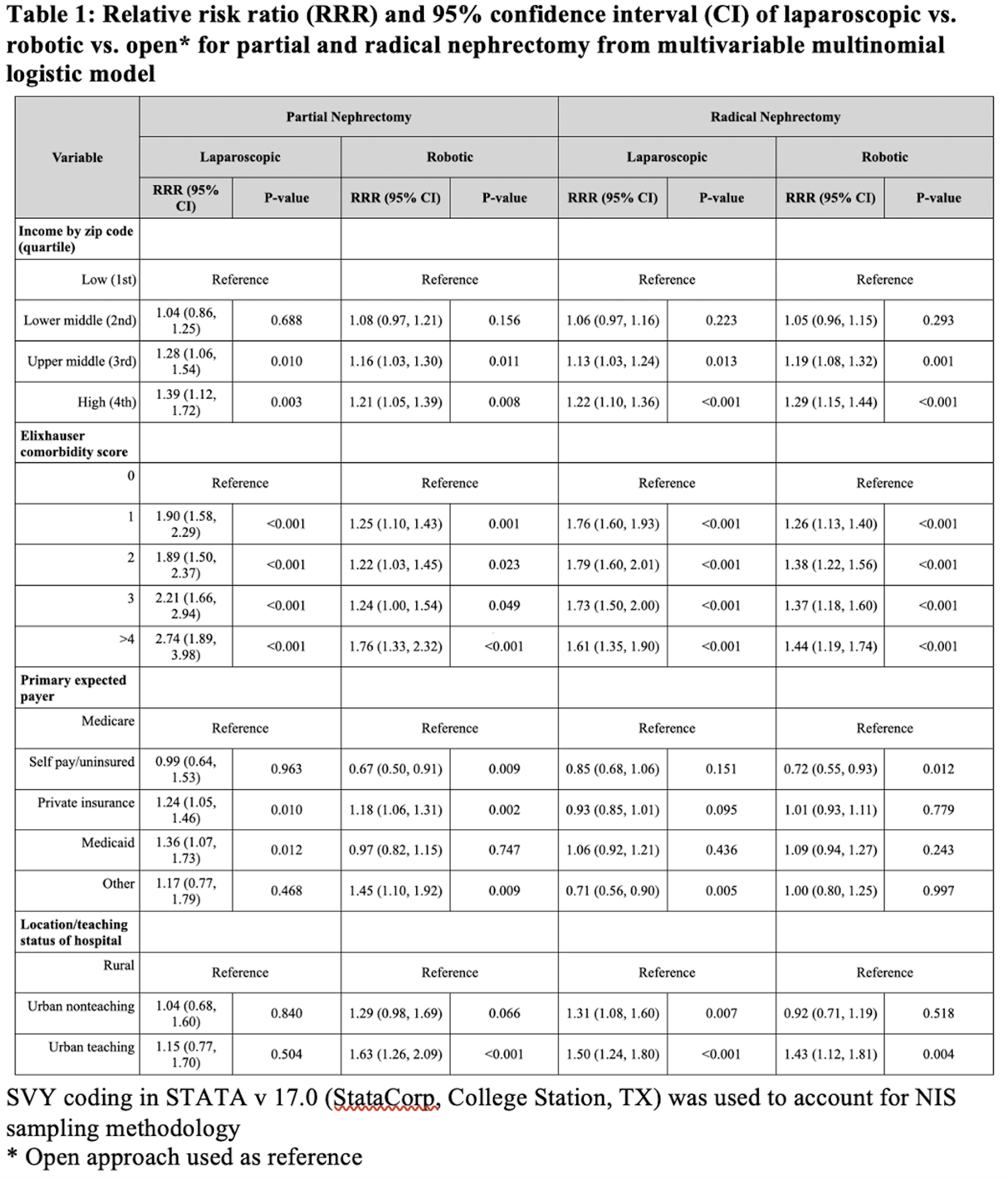
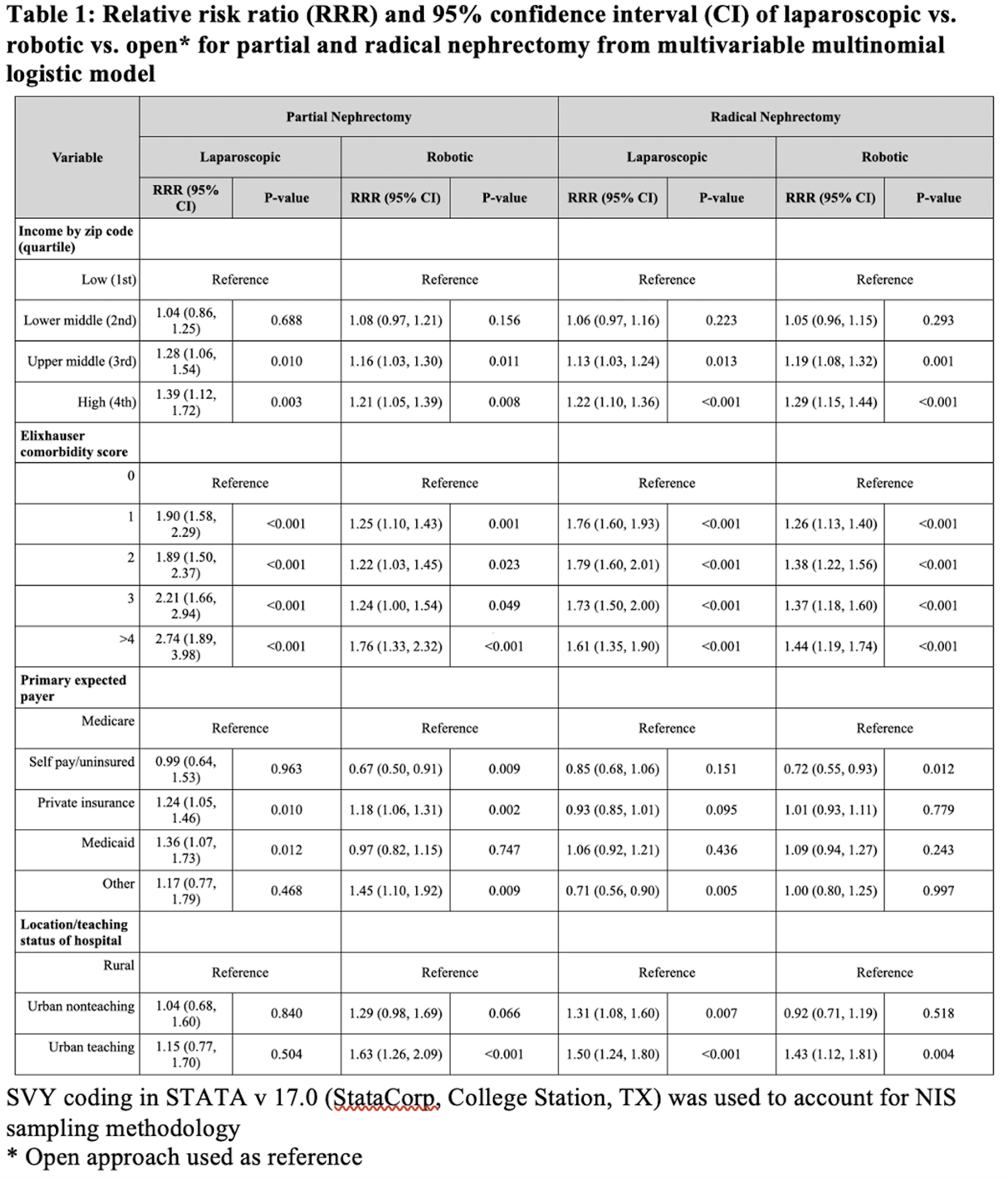
Results: In the PN group, 4,543 (28.5%) were treated with open PN (OPN), 1,515 (9.52%) with laparoscopic PN (LPN), and 9,857 (61.9%) with robotic PN (RPN). In the RN group, 11,588 (48.1%) were treated with open RN (ORN), 6,533 (27.1%) with laparoscopic RN (LRN), and 5,947 (24.7%) with robotic RN (RRN). There was an increase in robotic and laparoscopic surgery and decrease in open surgery over the study period for both PN and RN (P <0.001). For PN, multivariable analysis (Table 1) showed higher income quartile, private insurance coverage, and treatment at urban teaching facilities to be associated with higher likelihood of receiving MIS compared to OPN. For RN, high income quartile and treatment at urban teaching facilities were associated with higher likelihood of receiving MIS compared to ORN. Self pay/uninsured patients are less likely to receive both RPN and RRN.
Conclusions: There was increased MIS utilization for nephrectomy with a concurrent decrease in open surgery over the studied period. RRN and RPN use is significantly higher at urban teaching facilities. Patients with higher comorbidity burden are more likely to undergo MIS. Uninsured patients are less likely to have access to robotic nephrectomy. SOURCE OF
Funding: Sanjana Ranganathan is a Burroughs Wellcome Fund Scholar supported by a Burroughs Wellcome Fund Physician Scientist Institutional Award to the Texas A&M University Academy of Physician Scientists.
Podium Session
Session: PD40: Kidney Cancer: Localized: Surgical Therapy IV
PD40-01: Trends in Open, Laparoscopic, and Robotic Approach for Partial and Radical Nephrectomy for Renal Cancer: A Real-World Study Using the National Inpatient Sample Database
Monday, May 1, 2023
7:00 AM – 7:10 AM CST
Location: S404A
- SR
Podium Presenter(s)
Introduction: Partial nephrectomy (PN) is a preferred option for management of small renal masses due to benefits in postoperative renal function offered by preservation of normal parenchyma when compared to radical nephrectomy (RN). PN is a technically challenging procedure, requiring a high level of expertise to achieve negative margins and minimize blood loss and ischemia times. Considering increased interest in minimally invasive surgery (MIS) and the rapid adoption of robotic surgery within the field of urology, our study aims to elucidate contemporary trends in surgical approach for PN and RN and analyze patient and facility characteristics associated with treatment choice.
Methods: We used the National Inpatient Sample to identify patients diagnosed with malignant neoplasm of the kidney treated with PN or RN from 2014 to 2019. We examined trends in surgical approach (open, laparoscopic, and robotic) over the study period using a Wilcoxon-type test for trend and performed multivariable logistic regression modeling to determine relevant covariates.
Results: In the PN group, 4,543 (28.5%) were treated with open PN (OPN), 1,515 (9.52%) with laparoscopic PN (LPN), and 9,857 (61.9%) with robotic PN (RPN). In the RN group, 11,588 (48.1%) were treated with open RN (ORN), 6,533 (27.1%) with laparoscopic RN (LRN), and 5,947 (24.7%) with robotic RN (RRN). There was an increase in robotic and laparoscopic surgery and decrease in open surgery over the study period for both PN and RN (P <0.001). For PN, multivariable analysis (Table 1) showed higher income quartile, private insurance coverage, and treatment at urban teaching facilities to be associated with higher likelihood of receiving MIS compared to OPN. For RN, high income quartile and treatment at urban teaching facilities were associated with higher likelihood of receiving MIS compared to ORN. Self pay/uninsured patients are less likely to receive both RPN and RRN.
Conclusions: There was increased MIS utilization for nephrectomy with a concurrent decrease in open surgery over the studied period. RRN and RPN use is significantly higher at urban teaching facilities. Patients with higher comorbidity burden are more likely to undergo MIS. Uninsured patients are less likely to have access to robotic nephrectomy. SOURCE OF
Funding: Sanjana Ranganathan is a Burroughs Wellcome Fund Scholar supported by a Burroughs Wellcome Fund Physician Scientist Institutional Award to the Texas A&M University Academy of Physician Scientists.