Back
Introduction: Patients with increasing comorbidities are at risk of poor postoperative outcomes. Comorbidity indices have been developed to identify high-risk patients; the most common include the Charlson Comorbidity Index (CCI), Elixhauser/Van Walraven Index (VWI), and modified frailty index (mFI). This study compares the ability of these indices to predict adverse events after inflatable penile prosthesis (IPP) and artificial urinary sphincter (AUS) placement.
Methods: Using the State Inpatient Database (SID) and State Ambulatory Surgery and Services Database (SASD) for Florida (FL) from 2010-2015 and for California (CA) from 2010-2011, we identified patients who underwent IPP or AUS placement. CCI, VWI, and mFI were calculated for each patient. We extracted 30-day ER services, 30-day inpatient readmissions, 90-day postoperative complications, and 90-day device complications. We constructed receiver operating characteristic curves and compared area under the curve (AUC) between the comorbidity indices.
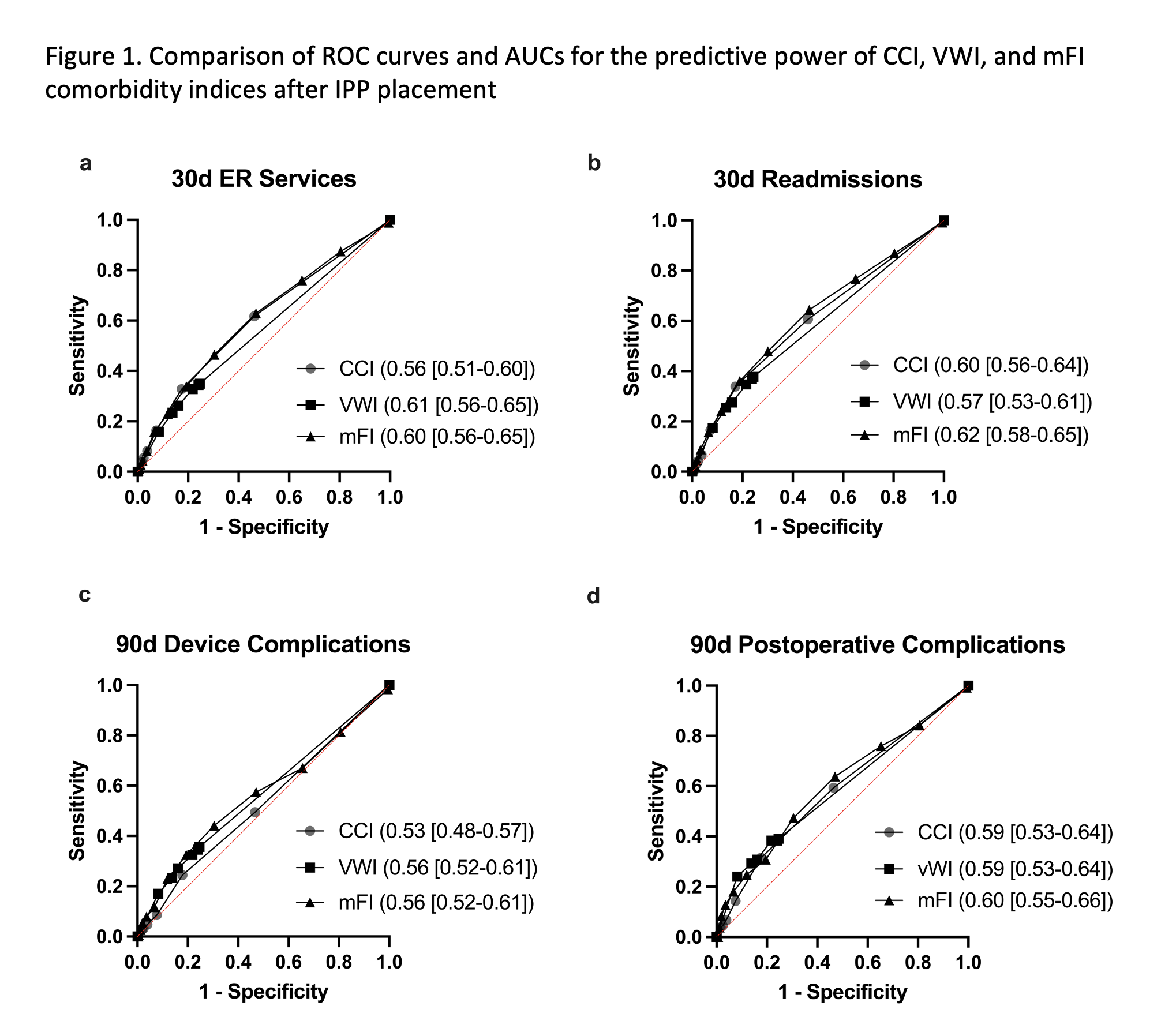
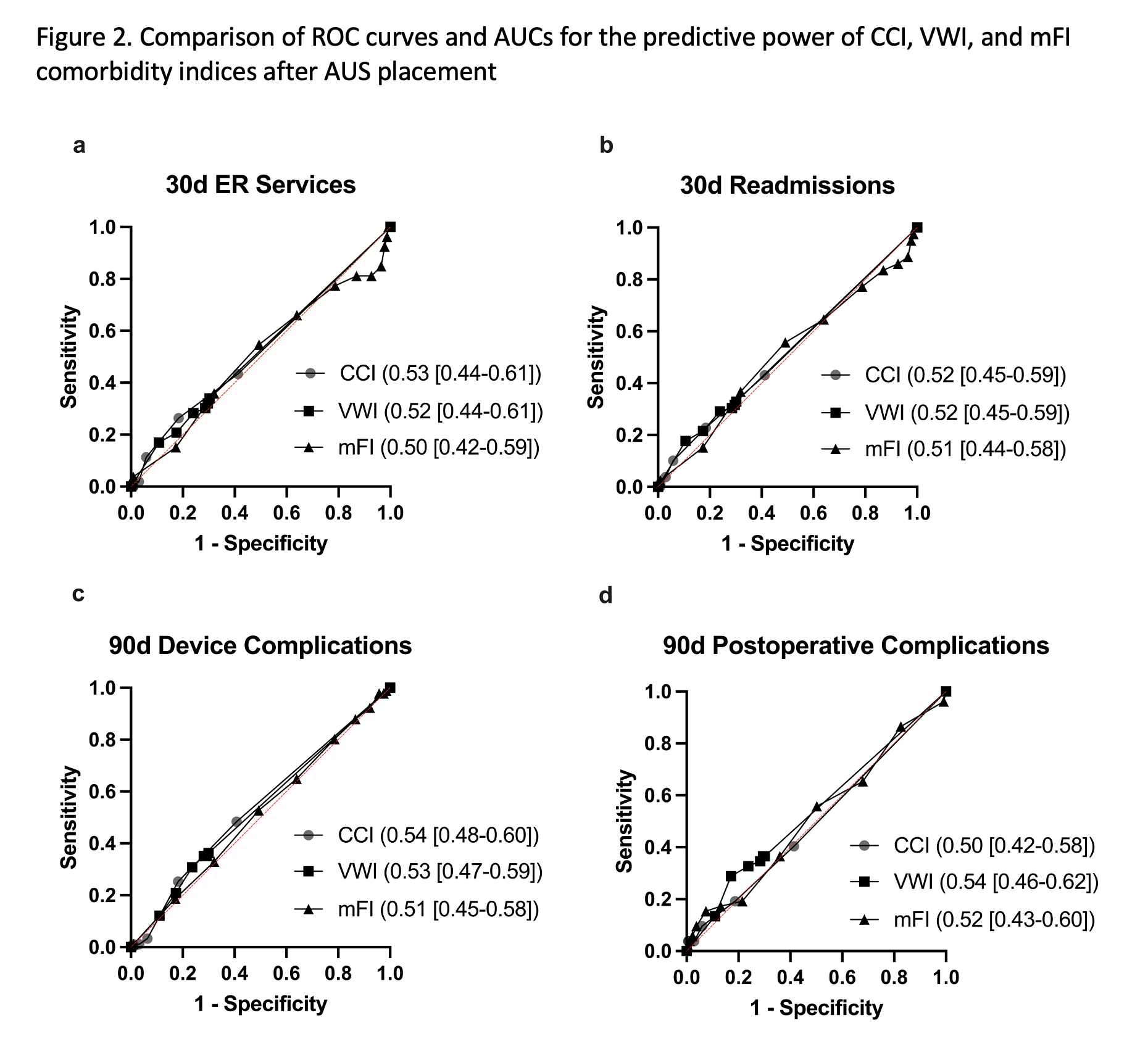
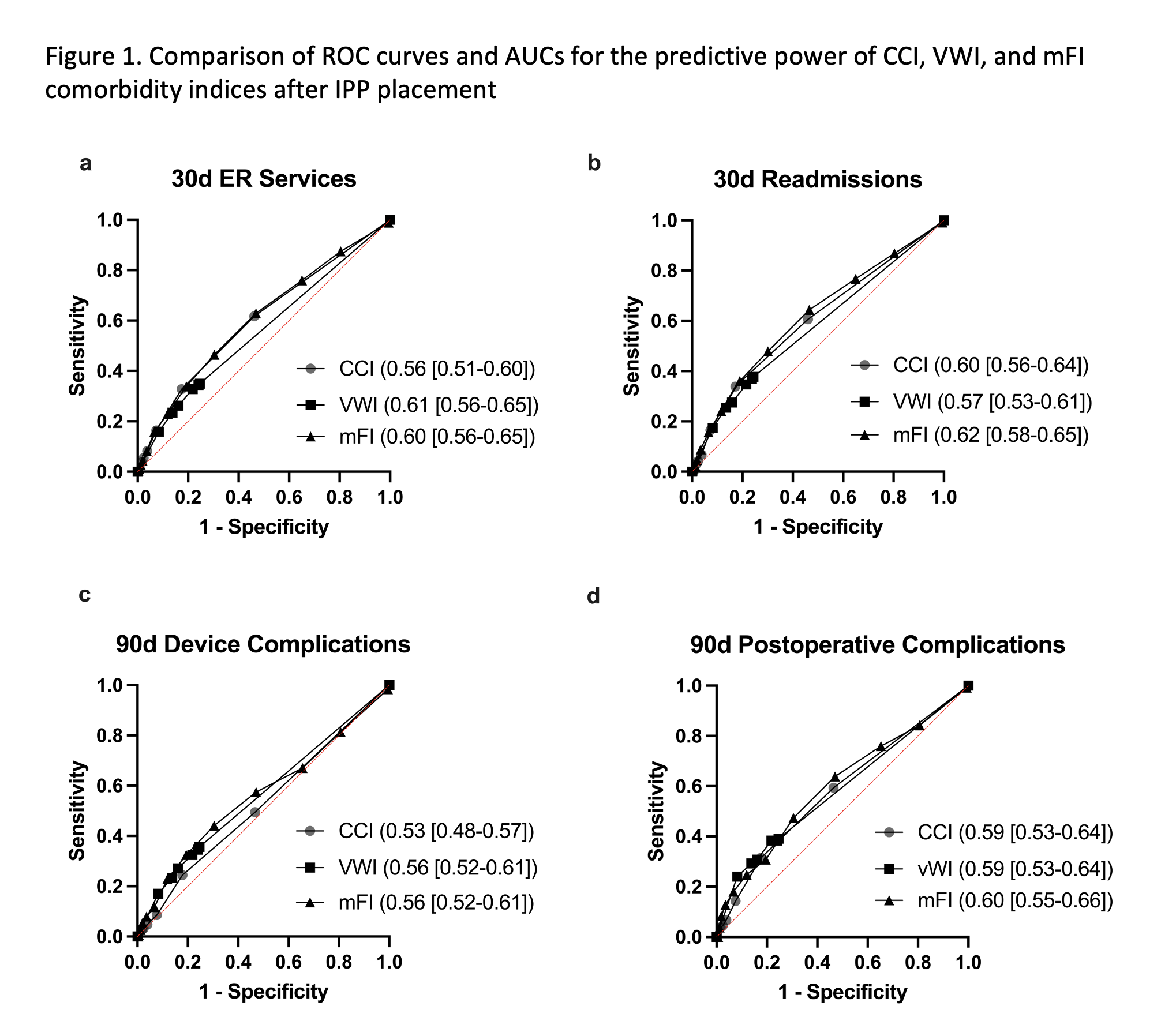
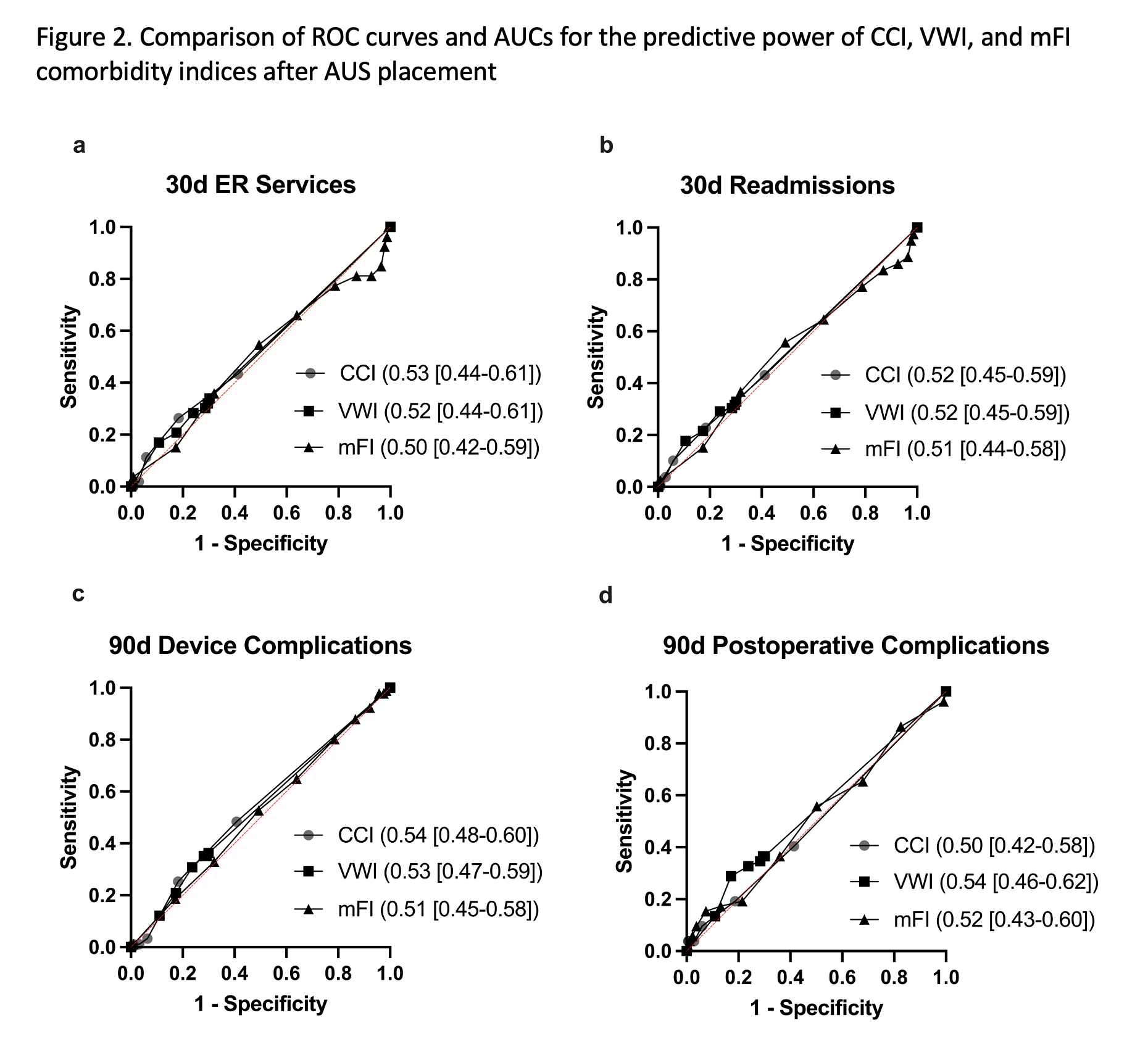
Results: We identified 4242 IPP patients (3060 from FL and 1181 from CA) and 1190 AUS patients (705 from FL and 485 from CA). 4.4% of IPP patients and 7.6% of AUS patients had a device complication. All three comorbidity indices had poor performance in predicting postoperative outcomes. All AUCs and their 95% CIs were less than 0.70. The CCI was the weakest predictor of 30-day ER services (AUC=0.56, 95% CI [0.51-0.60] for IPP) while the VWI was weakest for 30-day readmissions (AUC=0.57, 95% CI [0.53-0.61] for IPP) (Figure 1). All indices had better performance for IPP patients compared to AUS patients (Figure 2). These findings were consistent when analyzing each state individually.
Conclusions: All three commonly used comorbidity indices had poor predictive ability of adverse outcomes following IPP or AUS implantation. Our results support the need for further research and development of a urology-specific comorbidity index to better identify high-risk patients. SOURCE OF
Funding: None
Moderated Poster Session
Session: MP62: Sexual Function/Dysfunction: Surgical Therapy I
MP62-17: The Evaluation of Three Validated Comorbidity Indices to Predict Postoperative Outcomes after Inflatable Penile Prosthesis and Artificial Urinary Sphincter Placement: Which is Best?
Sunday, April 30, 2023
1:00 PM – 3:00 PM CST
Location: S404C
- MT
Michael Tram, BA
Albany Medical Center
Poster Presenter(s)
Introduction: Patients with increasing comorbidities are at risk of poor postoperative outcomes. Comorbidity indices have been developed to identify high-risk patients; the most common include the Charlson Comorbidity Index (CCI), Elixhauser/Van Walraven Index (VWI), and modified frailty index (mFI). This study compares the ability of these indices to predict adverse events after inflatable penile prosthesis (IPP) and artificial urinary sphincter (AUS) placement.
Methods: Using the State Inpatient Database (SID) and State Ambulatory Surgery and Services Database (SASD) for Florida (FL) from 2010-2015 and for California (CA) from 2010-2011, we identified patients who underwent IPP or AUS placement. CCI, VWI, and mFI were calculated for each patient. We extracted 30-day ER services, 30-day inpatient readmissions, 90-day postoperative complications, and 90-day device complications. We constructed receiver operating characteristic curves and compared area under the curve (AUC) between the comorbidity indices.
Results: We identified 4242 IPP patients (3060 from FL and 1181 from CA) and 1190 AUS patients (705 from FL and 485 from CA). 4.4% of IPP patients and 7.6% of AUS patients had a device complication. All three comorbidity indices had poor performance in predicting postoperative outcomes. All AUCs and their 95% CIs were less than 0.70. The CCI was the weakest predictor of 30-day ER services (AUC=0.56, 95% CI [0.51-0.60] for IPP) while the VWI was weakest for 30-day readmissions (AUC=0.57, 95% CI [0.53-0.61] for IPP) (Figure 1). All indices had better performance for IPP patients compared to AUS patients (Figure 2). These findings were consistent when analyzing each state individually.
Conclusions: All three commonly used comorbidity indices had poor predictive ability of adverse outcomes following IPP or AUS implantation. Our results support the need for further research and development of a urology-specific comorbidity index to better identify high-risk patients. SOURCE OF
Funding: None