Back
Introduction: Approximately 10,000 patients undergo cystectomy with ileal conduit diversion annually in the USA, of which ~ 50% will subsequently develop a parastomal hernia (PSH) at 2 years. Despite this, no well-established “best” practice for stoma creation exists. Due to the knowledge gap between urostomy surgical factors and abdominal wall forces, we developed a silicone and ex-vivo porcine fascia-based model for study. Our objective was to measure the relationship between incision size/type/material and axial tension force (ATF) as a surrogate for herniation force. This model was then used to evaluate a clinically applicable prevention strategy.
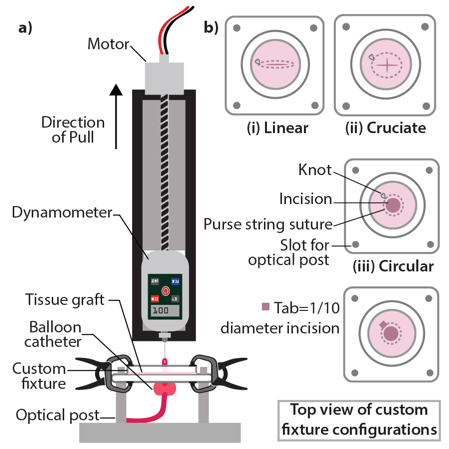
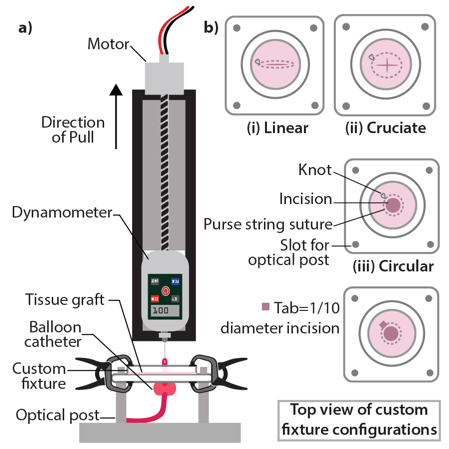
Methods: See system in Fig. 1a. Using incisions (linear, cruciate, circular) ranging from 1 to 3 cm (0.5cm increments) in 0.5mm silicone sheets, a dynamometer was hooked to a Foley catheter at the drainage aperture. Balloons were hydrated to 125% incision dimension. Upward ATF was recorded until balloon herniation and repeated up to N=5 membranes/size. Clinically applicable sized fascia was then used. To test force with suture, 4-0 Nylon purse string suture 1.5mm from incision edge were used (1b). A plastic tab 10% of incision diameter was laid while tying suture to prevent incisional constriction.
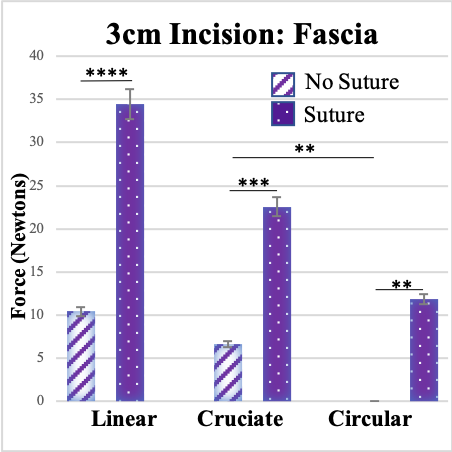
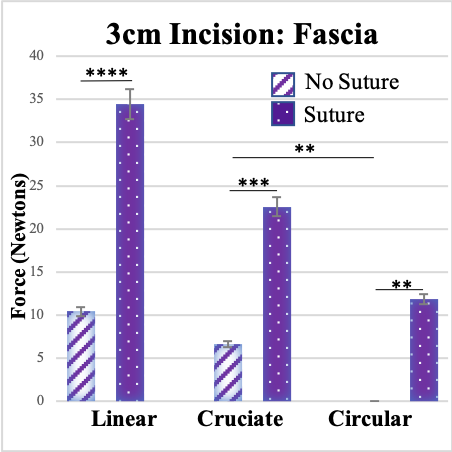
Results: The silicone ATF for herniation varied widely by incision type (Range 2.36 – 35.05 N). Linear ATF was highest, matched for size. Cruciate ATF was significantly higher than circular for each size. 3 cm incisions in ex vivo porcine fascia (Fig. 2) performed similarly. Suture reinforcement significantly raised herniation ATF for all incision types in both silicone and fascia. For example, for 3 cm cruciate, suture increased ATF 2.4-fold in silicone (p=0.008) and 3.3-fold in fascia (p=0.0001, Fig. 2).
Conclusions: This ex-vivo study suggests incision type, size, and suture reinforcement have predictable influences on ATF for herniation. En-bloc porcine and cadaveric human studies are underway to assessing these factors in more clinically optimized models. If confirmed, these data may be used to standardize urostomy creation, reducing PSH risk. SOURCE OF
Funding: American Urology Association, Urology Care Foundation Research Award
Moderated Poster Session
Session: MP65: Trauma/Reconstruction/Diversion: Augmentation, Substitution, Diversion
MP65-03: Assessment of Urostomy Parastomal Herniation Forces and Prevention Strategies
Sunday, April 30, 2023
1:00 PM – 3:00 PM CST
Location: S505

Diboro L. Kanabolo, MD (he/him/his)
University of Washington
Poster Presenter(s)
Introduction: Approximately 10,000 patients undergo cystectomy with ileal conduit diversion annually in the USA, of which ~ 50% will subsequently develop a parastomal hernia (PSH) at 2 years. Despite this, no well-established “best” practice for stoma creation exists. Due to the knowledge gap between urostomy surgical factors and abdominal wall forces, we developed a silicone and ex-vivo porcine fascia-based model for study. Our objective was to measure the relationship between incision size/type/material and axial tension force (ATF) as a surrogate for herniation force. This model was then used to evaluate a clinically applicable prevention strategy.
Methods: See system in Fig. 1a. Using incisions (linear, cruciate, circular) ranging from 1 to 3 cm (0.5cm increments) in 0.5mm silicone sheets, a dynamometer was hooked to a Foley catheter at the drainage aperture. Balloons were hydrated to 125% incision dimension. Upward ATF was recorded until balloon herniation and repeated up to N=5 membranes/size. Clinically applicable sized fascia was then used. To test force with suture, 4-0 Nylon purse string suture 1.5mm from incision edge were used (1b). A plastic tab 10% of incision diameter was laid while tying suture to prevent incisional constriction.
Results: The silicone ATF for herniation varied widely by incision type (Range 2.36 – 35.05 N). Linear ATF was highest, matched for size. Cruciate ATF was significantly higher than circular for each size. 3 cm incisions in ex vivo porcine fascia (Fig. 2) performed similarly. Suture reinforcement significantly raised herniation ATF for all incision types in both silicone and fascia. For example, for 3 cm cruciate, suture increased ATF 2.4-fold in silicone (p=0.008) and 3.3-fold in fascia (p=0.0001, Fig. 2).
Conclusions: This ex-vivo study suggests incision type, size, and suture reinforcement have predictable influences on ATF for herniation. En-bloc porcine and cadaveric human studies are underway to assessing these factors in more clinically optimized models. If confirmed, these data may be used to standardize urostomy creation, reducing PSH risk. SOURCE OF
Funding: American Urology Association, Urology Care Foundation Research Award