Back
Introduction: True local recurrence (LR) in the partial nephrectomy (PN) bed is uncommon, with reported rates of 1-3%. To date, there is sparse literature examining oncologic outcomes in this population. Our study seeks to define oncologic outcomes and determine if there is an association of LR with distant metastasis and cancer-specific survival (CSS).
Methods: We identified 2,164 adults treated with PN for unilateral, sporadic, localized (M0) renal cell carcinoma (RCC) from 2000 to 2019. LR was defined as new enhancing tumor growth within the PN bed on MRI or CT. Survival rates were estimated using the Kaplan-Meier method. Associations with death from RCC following PN were evaluated using Cox proportional hazards regression models. The association of LR with CSS was analyzed in the subset of patients with clear cell RCC.
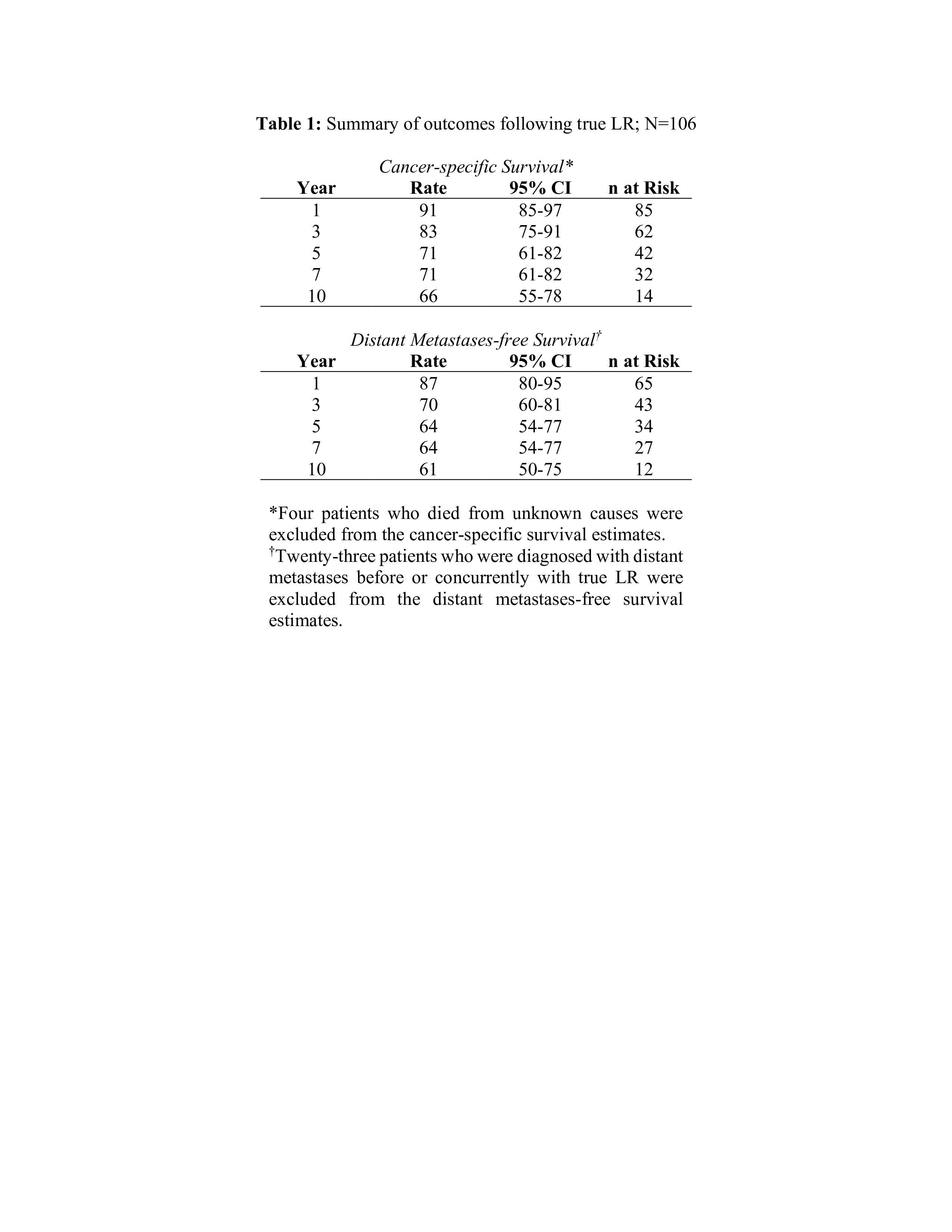
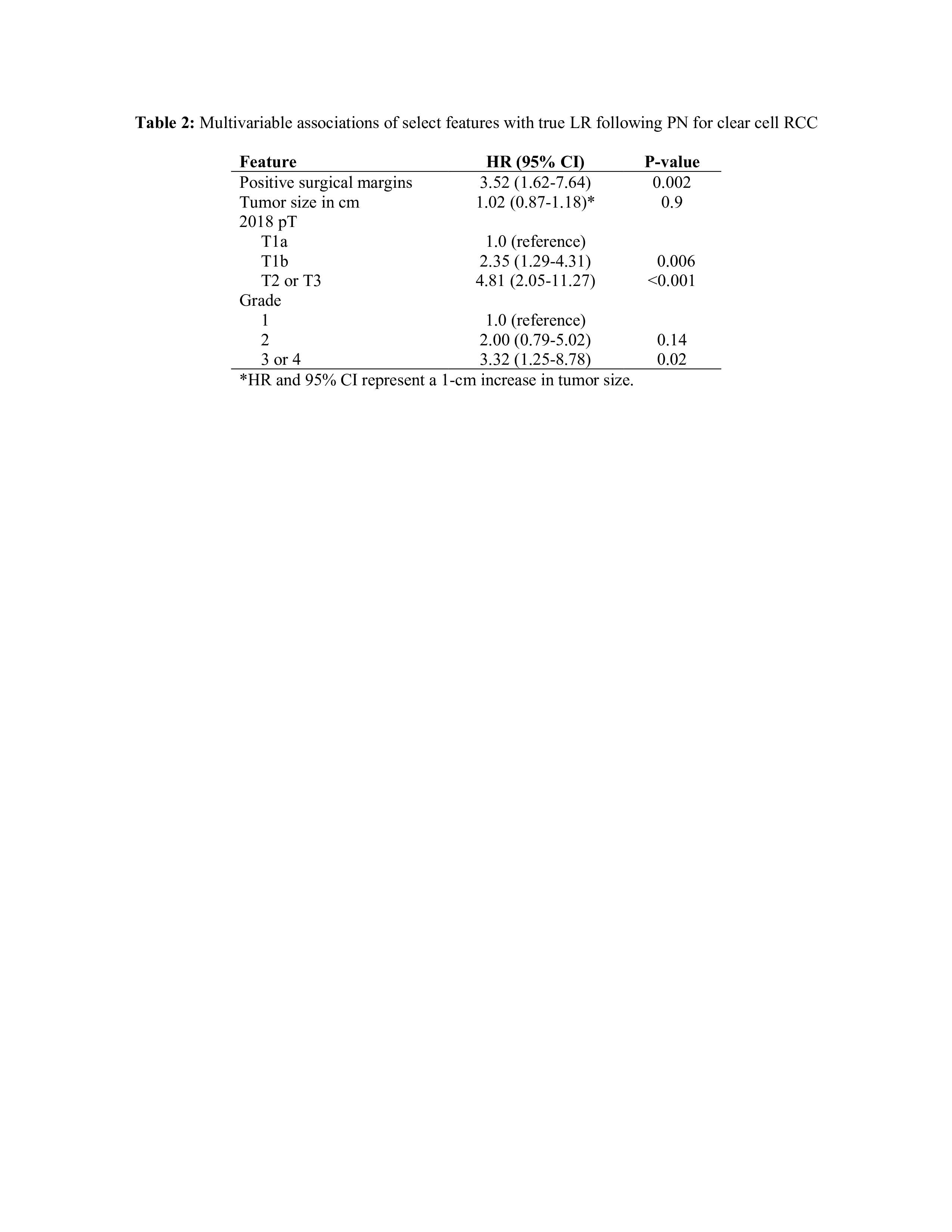
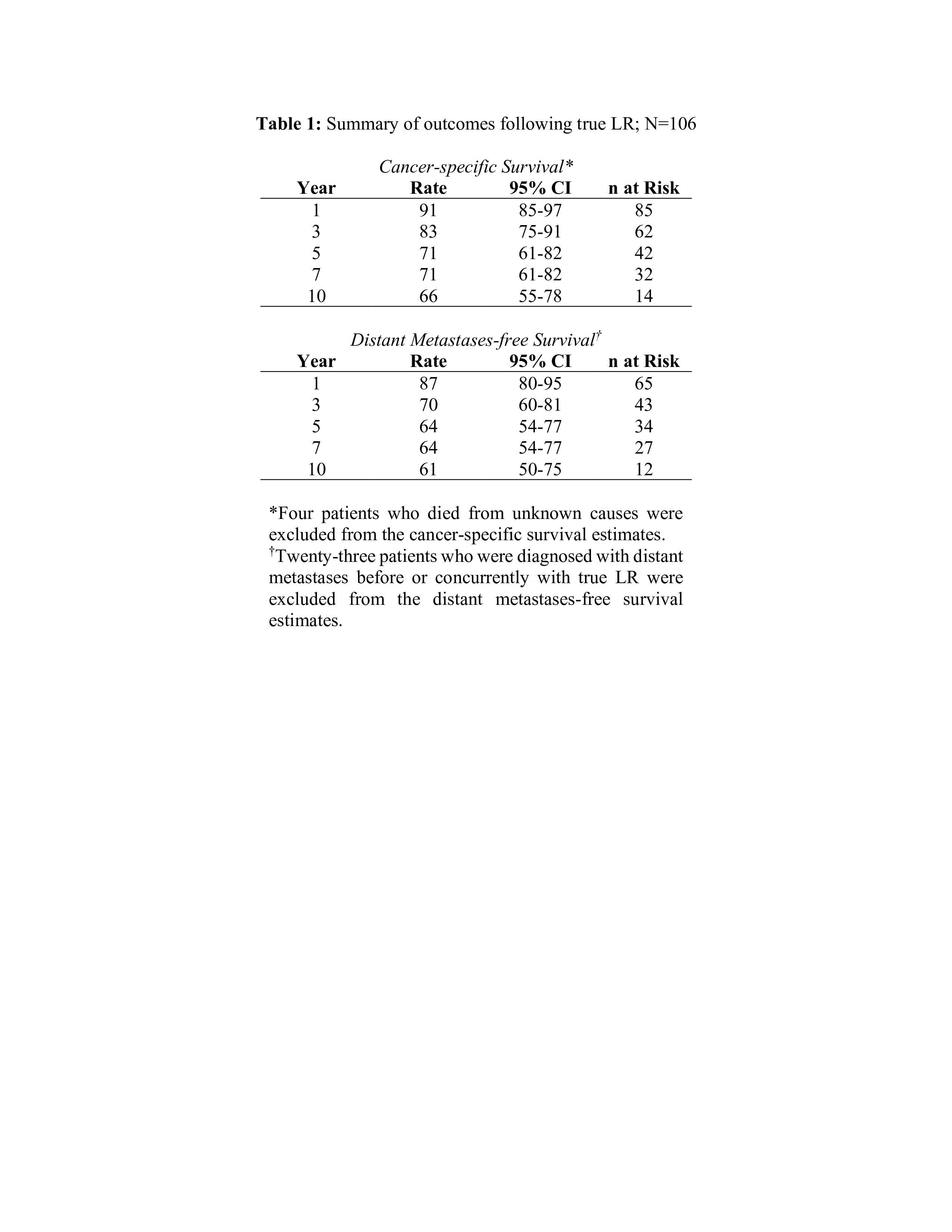
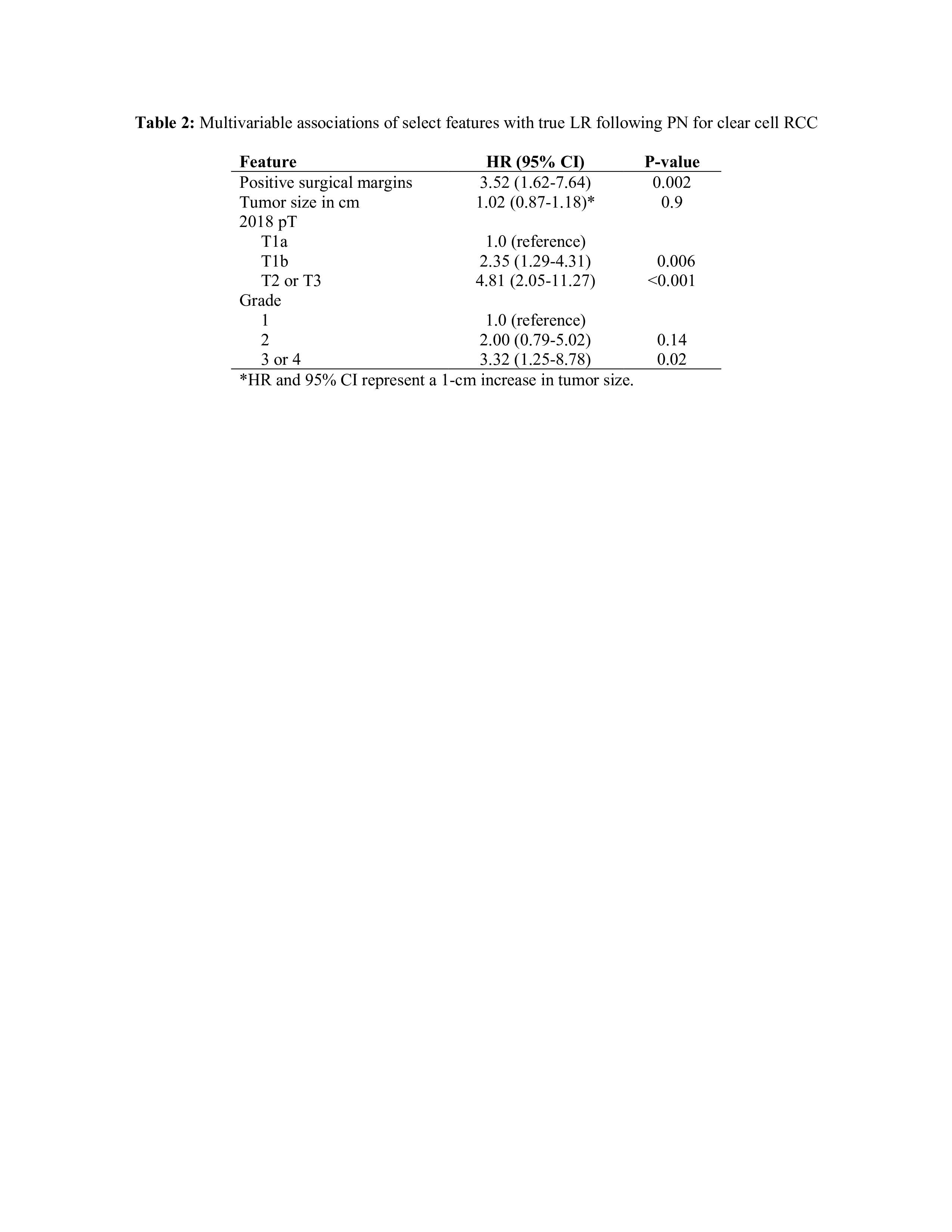
Results: A total of 106 true LR were identified. Median time to LR was 3.3 years (IQR 1.7-5.1). Management of LR included 89 surgeries, 5 systemic therapy, 4 surveillance, 8 others. Forty-five patients died at a median of 3.5 years (IQR 1.6-5.3), including 26 from RCC at a median of 1.9 years (IQR 0.8-4.0). Median duration of post-recurrence follow-up was 5.1 years (IQR 2.3-9.1). Among 83 patients who remained M0 at LR, 26 subsequently developed metastases at a median of 1.5 years (IQR 0.3-2.4). Estimated MFS and CSS following LR are summarized in Table 1. When analyzed as a time-dependent covariate, LR was associated with death from RCC following PN (HR 12.45; 95% CI 6.65-23.31; p<0.001), and after adjusting for tumor size, pT classification, and grade, LR was associated with development of metastasis (HR 6.25; 95% CI 3.5-11; p<0.001). When adjusting for metastasis, LR remained significantly associated with risk of death from RCC (HR 1.93; 95% CI 1.07-3.50; p=0.03). Multivariable associations of select features with LR in the clear cell RCC cohort are presented in Table 2.
Conclusions: True LR is uncommon and is associated with adverse pathologic features including high stage and grade, histology, and margin status. Our data suggests aggressive management of LR may prevent metastasis and RCC related death. SOURCE OF
Funding: NA
Moderated Poster Session
Session: MP58: Kidney Cancer: Localized: Surgical Therapy III
MP58-09: True Local Recurrence Following Partial Nephrectomy
Sunday, April 30, 2023
9:30 AM – 11:30 AM CST
Location: S504
- CB
Cameron Britton, MD, BS
Mayo Clinic, Rochester
Poster Presenter(s)
Introduction: True local recurrence (LR) in the partial nephrectomy (PN) bed is uncommon, with reported rates of 1-3%. To date, there is sparse literature examining oncologic outcomes in this population. Our study seeks to define oncologic outcomes and determine if there is an association of LR with distant metastasis and cancer-specific survival (CSS).
Methods: We identified 2,164 adults treated with PN for unilateral, sporadic, localized (M0) renal cell carcinoma (RCC) from 2000 to 2019. LR was defined as new enhancing tumor growth within the PN bed on MRI or CT. Survival rates were estimated using the Kaplan-Meier method. Associations with death from RCC following PN were evaluated using Cox proportional hazards regression models. The association of LR with CSS was analyzed in the subset of patients with clear cell RCC.
Results: A total of 106 true LR were identified. Median time to LR was 3.3 years (IQR 1.7-5.1). Management of LR included 89 surgeries, 5 systemic therapy, 4 surveillance, 8 others. Forty-five patients died at a median of 3.5 years (IQR 1.6-5.3), including 26 from RCC at a median of 1.9 years (IQR 0.8-4.0). Median duration of post-recurrence follow-up was 5.1 years (IQR 2.3-9.1). Among 83 patients who remained M0 at LR, 26 subsequently developed metastases at a median of 1.5 years (IQR 0.3-2.4). Estimated MFS and CSS following LR are summarized in Table 1. When analyzed as a time-dependent covariate, LR was associated with death from RCC following PN (HR 12.45; 95% CI 6.65-23.31; p<0.001), and after adjusting for tumor size, pT classification, and grade, LR was associated with development of metastasis (HR 6.25; 95% CI 3.5-11; p<0.001). When adjusting for metastasis, LR remained significantly associated with risk of death from RCC (HR 1.93; 95% CI 1.07-3.50; p=0.03). Multivariable associations of select features with LR in the clear cell RCC cohort are presented in Table 2.
Conclusions: True LR is uncommon and is associated with adverse pathologic features including high stage and grade, histology, and margin status. Our data suggests aggressive management of LR may prevent metastasis and RCC related death. SOURCE OF
Funding: NA