Back
Introduction: Urinary incontinence (UI) is highly prevalent in low- and middle-income countries (LMIC). Concurrently, the availability of surgical or conservative UI treatments in LMIC is limited
Methods: We conducted a prospective feasibility study of women in Belize with UI treated with pelvic floor physical therapy (PFPT) and education (PFE). This study is part of a larger initiative to establish a PFPT program in Belize in conjunction with the charity Global Surgical Expedition. Patients were recruited during a 7-day visiting trip. Enrolled patients received individual PFPT/PFE over the course 2 days (1 hour per day), consisting of biofeedback-enhanced PFMT including pelvic floor activation training (dynamic and functional activities) in addition to behavioral, dietary, and general pelvic education. Patients then completed a daily 6-month home regimen including 7 PFMT exercises (total 70 repetitions) comprising both endurance and quick flick exercises across supine, seated, and standing positions. Patients also performed comprehensive dietary and behavioral modification activities. Comprehensive outcomes were assessed at baseline and 6-months, including validated symptom (ICIQ-FLUTS) and QOL (IIQ-7) questionnaires, strength testing (PEFECT score, perineometry), and items assessing PFPT comprehension.
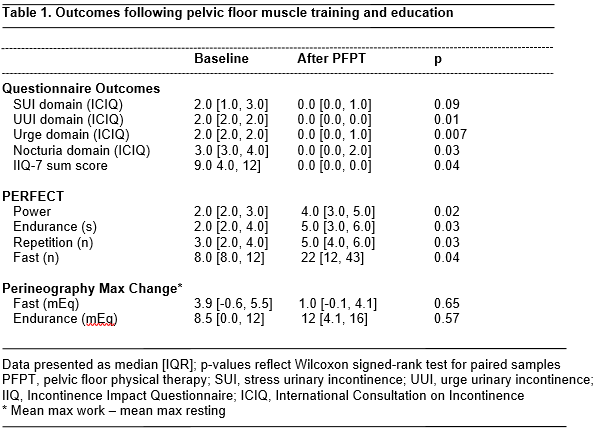
Results: Ten patients were enrolled and underwent baseline PFMT. One patient was lost to follow-up, leaving nine patients for interim analysis. The mean patient age, BMI, and parity were 51.4 (?6.6) years, 30.9 (?6.3), and 2.7 (?1.5). The mean duration of UI was 104.7 (?92.2) months. Provider assessment demonstrated patient comprehension of basic, endurance, and quick flick pelvic floor contractions in 9 (100%), 8 (89%), and 7 (78%) patients, respectively. At 6-month follow-up, significant improvements were seen across validated questionnaire and strength measurement assessments (Table 1). Patient reported improvement level was 8.1 (?1.6) on a 10-point Likert scale.
Conclusions: Our interim analysis demonstrates that women in Belize demonstrate good understanding of PFMT/PFE. In addition, women in our study demonstrated significant improvements across subjective incontinence and QOL outcomes, as well as strength testing. Study recruitment is ongoing as part of a scaled effort to develop pelvic floor services in Belize. SOURCE OF
Funding: University of Virginia Center for Global Inquiry and Innovation; Global Surgical Expedition
Moderated Poster Session
Session: MP49: Global Health/Humanitarian
MP49-04: Pilot Pelvic Floor Therapy Program for the Treatment of Female Urinary Incontinence in Belize
Sunday, April 30, 2023
7:00 AM – 9:00 AM CST
Location: S401A
- FS
Poster Presenter(s)
Introduction: Urinary incontinence (UI) is highly prevalent in low- and middle-income countries (LMIC). Concurrently, the availability of surgical or conservative UI treatments in LMIC is limited
Methods: We conducted a prospective feasibility study of women in Belize with UI treated with pelvic floor physical therapy (PFPT) and education (PFE). This study is part of a larger initiative to establish a PFPT program in Belize in conjunction with the charity Global Surgical Expedition. Patients were recruited during a 7-day visiting trip. Enrolled patients received individual PFPT/PFE over the course 2 days (1 hour per day), consisting of biofeedback-enhanced PFMT including pelvic floor activation training (dynamic and functional activities) in addition to behavioral, dietary, and general pelvic education. Patients then completed a daily 6-month home regimen including 7 PFMT exercises (total 70 repetitions) comprising both endurance and quick flick exercises across supine, seated, and standing positions. Patients also performed comprehensive dietary and behavioral modification activities. Comprehensive outcomes were assessed at baseline and 6-months, including validated symptom (ICIQ-FLUTS) and QOL (IIQ-7) questionnaires, strength testing (PEFECT score, perineometry), and items assessing PFPT comprehension.
Results: Ten patients were enrolled and underwent baseline PFMT. One patient was lost to follow-up, leaving nine patients for interim analysis. The mean patient age, BMI, and parity were 51.4 (?6.6) years, 30.9 (?6.3), and 2.7 (?1.5). The mean duration of UI was 104.7 (?92.2) months. Provider assessment demonstrated patient comprehension of basic, endurance, and quick flick pelvic floor contractions in 9 (100%), 8 (89%), and 7 (78%) patients, respectively. At 6-month follow-up, significant improvements were seen across validated questionnaire and strength measurement assessments (Table 1). Patient reported improvement level was 8.1 (?1.6) on a 10-point Likert scale.
Conclusions: Our interim analysis demonstrates that women in Belize demonstrate good understanding of PFMT/PFE. In addition, women in our study demonstrated significant improvements across subjective incontinence and QOL outcomes, as well as strength testing. Study recruitment is ongoing as part of a scaled effort to develop pelvic floor services in Belize. SOURCE OF
Funding: University of Virginia Center for Global Inquiry and Innovation; Global Surgical Expedition
