Back
Introduction: Intradetrusor injection of onabotulinumtoxinA (BTX) is safe and efficacious in the treatment of neurogenic and non-neurogenic overactive bladder (OAB). Urinary tract infection (UTI) is a known potential adverse event. Published guidelines for cystoscopic procedures with manipulation recommend the use of prophylactic antibiotics, and prophylactic antibiotics are commonly administered pre-BTX. However, there is a paucity of data demonstrating that pre-procedural antibiotic administration decreases the rate of post-procedural UTI after BTX. In the era of antibiotic stewardship and avoidance of antibiotic overuse, we aimed to study the difference in UTI rates between patients asymptomatic for UTI who receive and do not receive antibiotics at the time of BTX in a prospective, randomized multi-institutional study. Here, we report our preliminary study results.
Methods: Patients with OAB undergoing BTX who were not symptomatic for UTI and had urinalysis demonstrating fewer than 2+ leukocyte esterase at the time of injection were randomized to receive either a single dose of pre-procedural prophylactic antibiotics or no antibiotics. Patients who had taken antibiotics within 48 hours of the procedure were excluded from study participation. Symptomatic UTIs within 2 weeks of injection was identified and recorded. Demographics and past medical history were recorded.
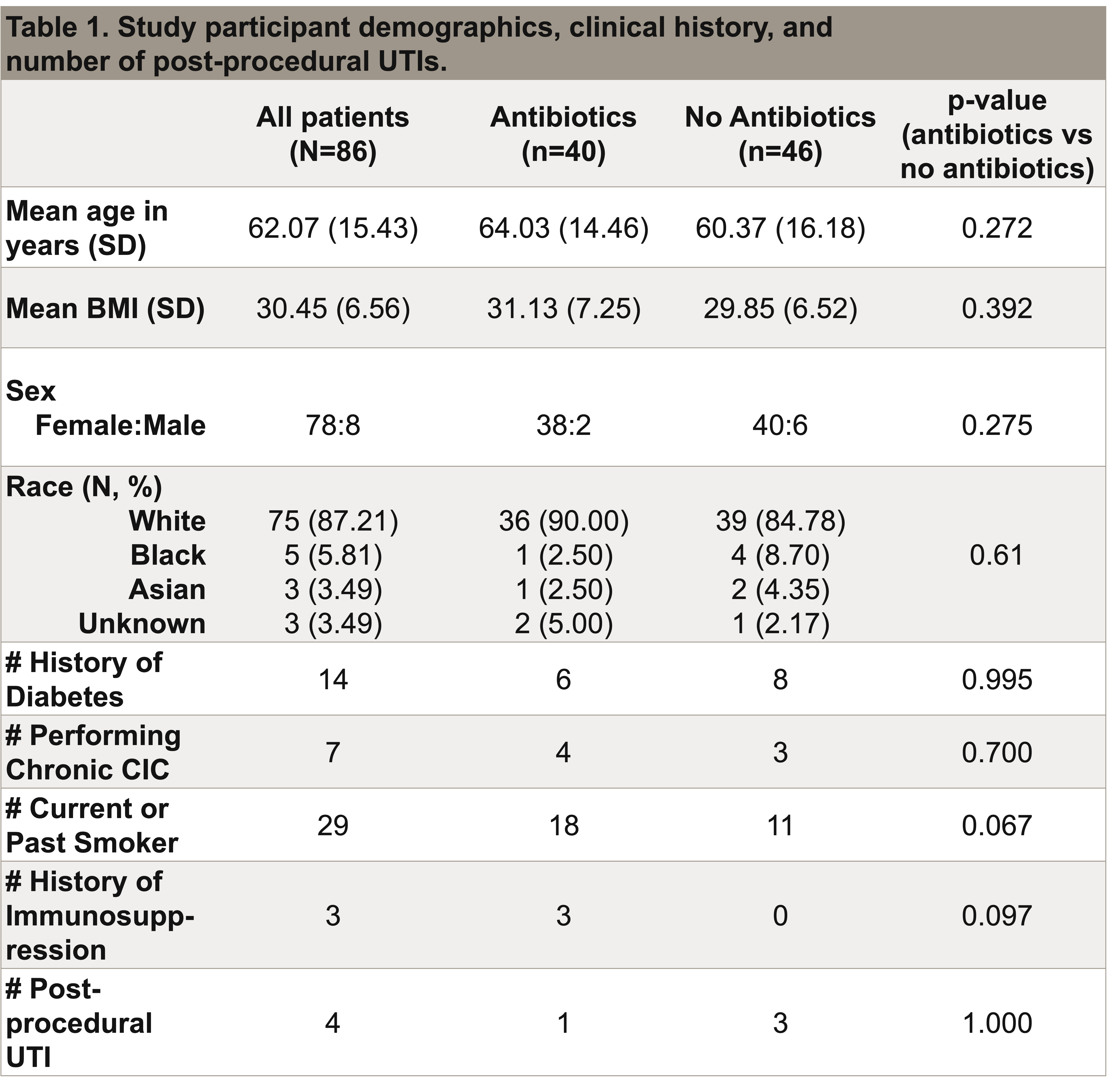
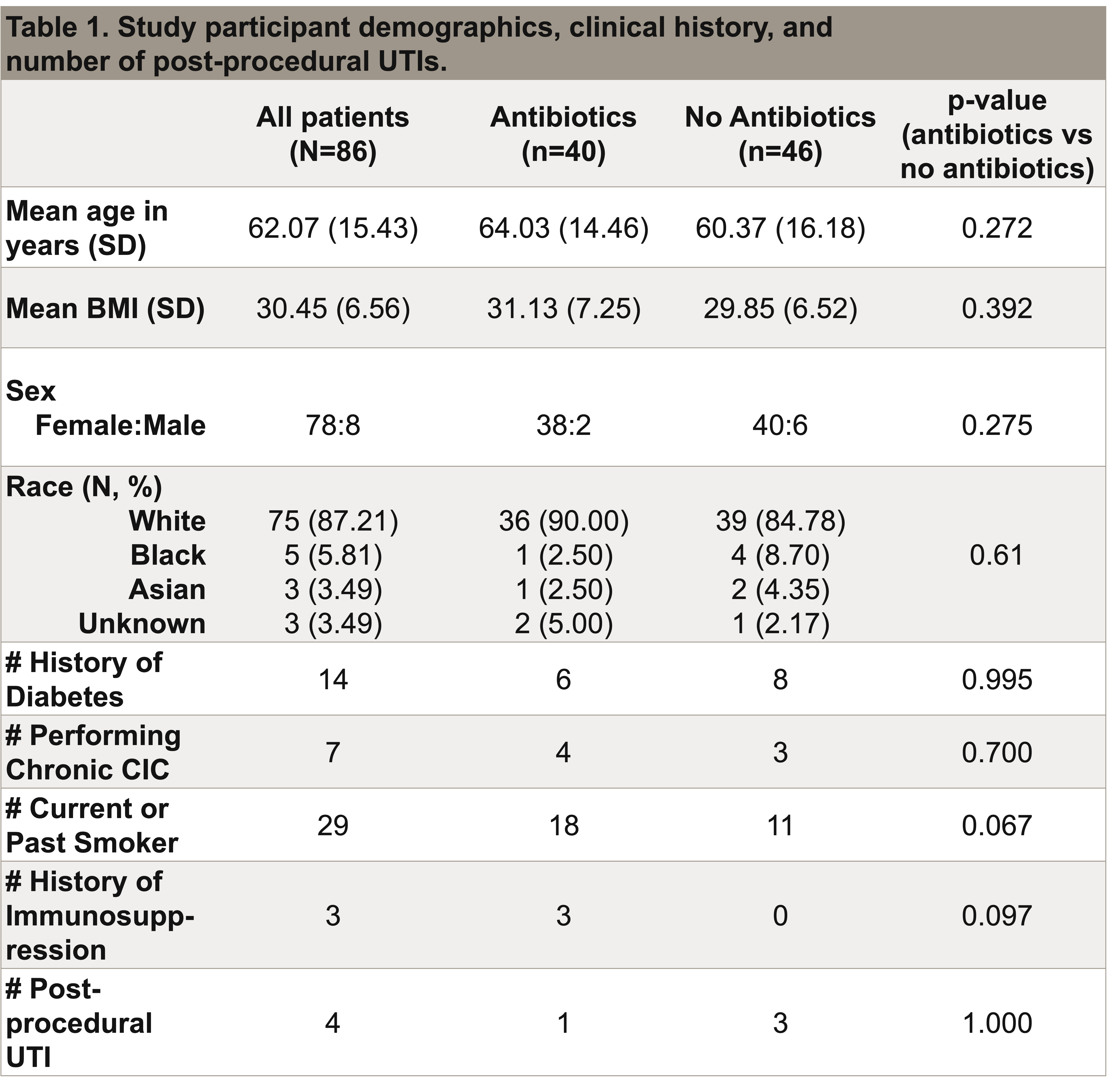
Results: Of 86 patients who have been enrolled, 40 were randomized to receive antibiotics, and 46 were randomized to not receive antibiotics. Table 1 summarizes the patient demographics, clinical history, and UTI rate. At 2-week follow up, a total of 4 patients developed UTI. One patient in the antibiotic group developed UTI, and 3 patients who did not receive antibiotics developed UTI.
Conclusions: Our preliminary results suggest that the use of a single dose of prophylactic antibiotic may not affect the rate of post-procedural UTI. Patient enrollment is ongoing to determine if these findings hold true in a larger patient cohort. SOURCE OF
Funding: 2020 Society of Urodynamics Female Pelvic Medicine & Urogenital Reconstruction Foundation Grant
Podium Session
Session: PD14: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Female Incontinence: Therapy I
PD14-04: Optimizing Antibiotic Use in the Treatment of Overactive Bladder: Evaluating the Need for Prophylactic Antibiotics Prior to OnabotulinumtoxinA Injection
Saturday, April 29, 2023
7:30 AM – 7:40 AM CST
Location: S501A
- JT
Justina Tam, MD
Stony Brook Medicine
Podium Presenter(s)
Introduction: Intradetrusor injection of onabotulinumtoxinA (BTX) is safe and efficacious in the treatment of neurogenic and non-neurogenic overactive bladder (OAB). Urinary tract infection (UTI) is a known potential adverse event. Published guidelines for cystoscopic procedures with manipulation recommend the use of prophylactic antibiotics, and prophylactic antibiotics are commonly administered pre-BTX. However, there is a paucity of data demonstrating that pre-procedural antibiotic administration decreases the rate of post-procedural UTI after BTX. In the era of antibiotic stewardship and avoidance of antibiotic overuse, we aimed to study the difference in UTI rates between patients asymptomatic for UTI who receive and do not receive antibiotics at the time of BTX in a prospective, randomized multi-institutional study. Here, we report our preliminary study results.
Methods: Patients with OAB undergoing BTX who were not symptomatic for UTI and had urinalysis demonstrating fewer than 2+ leukocyte esterase at the time of injection were randomized to receive either a single dose of pre-procedural prophylactic antibiotics or no antibiotics. Patients who had taken antibiotics within 48 hours of the procedure were excluded from study participation. Symptomatic UTIs within 2 weeks of injection was identified and recorded. Demographics and past medical history were recorded.
Results: Of 86 patients who have been enrolled, 40 were randomized to receive antibiotics, and 46 were randomized to not receive antibiotics. Table 1 summarizes the patient demographics, clinical history, and UTI rate. At 2-week follow up, a total of 4 patients developed UTI. One patient in the antibiotic group developed UTI, and 3 patients who did not receive antibiotics developed UTI.
Conclusions: Our preliminary results suggest that the use of a single dose of prophylactic antibiotic may not affect the rate of post-procedural UTI. Patient enrollment is ongoing to determine if these findings hold true in a larger patient cohort. SOURCE OF
Funding: 2020 Society of Urodynamics Female Pelvic Medicine & Urogenital Reconstruction Foundation Grant