Back
Introduction: Extended antibiotic prophylaxis after radical cystectomy (RC) reduces urinary tract infections (UTI) and urosepsis. Optimal duration of prophylaxis remains unknown as ureteral stents are associated with an increased risk of UTI. Similarly, the optimal duration and benefit of ureteral stents is unknown, with trends toward removing stents earlier or foregoing them altogether. Our protocol after RC previously consisted of ureteral stent duration of at least 14 days and 30 days of antibiotic prophylaxis postoperatively. To reduce stent duration and antibiotic exposure, we changed our protocol in 2020 to remove stents prior to discharge and stop antibiotic prophylaxis earlier (14d). We assessed rates of UTI and urine leak in our cohort of patients undergoing RC during this change.
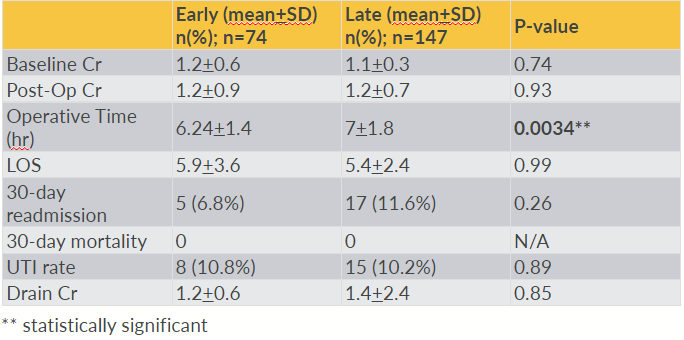
Methods: We performed a retrospective chart review of all patients who underwent radical cystectomy for bladder cancer at our institution between 2016-2022(OHSU IRB approved). Patients were stratified into early or late stent removal ( <14 or >14 days post-operatively). The primary outcomes were incidence of UTI (defined as positive urine culture requiring antibiotic treatment) and urine leak, as measured by postoperative drain creatinine measurement greater than twice serum creatinine Statisical analysis was performed using Wilcoxon test and chi-square analysis.
Results: Of 221 patients with evaluable data, 33% of patients had early and 67% had late stent removal. Mean day of stent removal was 8.0 versus 19.9 in the early versus late group. Antibiotic exposure was lower in the early stent removal group (10 vs 21 days, p= <0.05). There was no difference in rate of postoperative UTI when comparing early versus late stent removal (10.8% vs 10.2%, p=0.9). Similarly, there was no difference in rate of urine leak when comparing early versus late stent removal (0% vs 1.3%, p=0.31). Readmission rates were similar for early versus late stent removal (7 vs 12%, p=0.3).
Conclusions: Earlier stent removal and reduced duration of antibiotic prophylaxis after RC does not result in an increased rate of UTI or urine leak. Decreasing ureteral stent duration reduces postoperative antibiotic exposure without increasing adverse outcomes in patients undergoing RC. SOURCE OF
Funding: None
Moderated Poster Session
Session: MP32: Bladder Cancer: Invasive II
MP32-06: Early Stent Removal After Radical Cystectomy
Saturday, April 29, 2023
9:30 AM – 11:30 AM CST
Location: S403
- JW
Jessica Wenzel, MD
OHSU
Poster Presenter(s)
Introduction: Extended antibiotic prophylaxis after radical cystectomy (RC) reduces urinary tract infections (UTI) and urosepsis. Optimal duration of prophylaxis remains unknown as ureteral stents are associated with an increased risk of UTI. Similarly, the optimal duration and benefit of ureteral stents is unknown, with trends toward removing stents earlier or foregoing them altogether. Our protocol after RC previously consisted of ureteral stent duration of at least 14 days and 30 days of antibiotic prophylaxis postoperatively. To reduce stent duration and antibiotic exposure, we changed our protocol in 2020 to remove stents prior to discharge and stop antibiotic prophylaxis earlier (14d). We assessed rates of UTI and urine leak in our cohort of patients undergoing RC during this change.
Methods: We performed a retrospective chart review of all patients who underwent radical cystectomy for bladder cancer at our institution between 2016-2022(OHSU IRB approved). Patients were stratified into early or late stent removal ( <14 or >14 days post-operatively). The primary outcomes were incidence of UTI (defined as positive urine culture requiring antibiotic treatment) and urine leak, as measured by postoperative drain creatinine measurement greater than twice serum creatinine Statisical analysis was performed using Wilcoxon test and chi-square analysis.
Results: Of 221 patients with evaluable data, 33% of patients had early and 67% had late stent removal. Mean day of stent removal was 8.0 versus 19.9 in the early versus late group. Antibiotic exposure was lower in the early stent removal group (10 vs 21 days, p= <0.05). There was no difference in rate of postoperative UTI when comparing early versus late stent removal (10.8% vs 10.2%, p=0.9). Similarly, there was no difference in rate of urine leak when comparing early versus late stent removal (0% vs 1.3%, p=0.31). Readmission rates were similar for early versus late stent removal (7 vs 12%, p=0.3).
Conclusions: Earlier stent removal and reduced duration of antibiotic prophylaxis after RC does not result in an increased rate of UTI or urine leak. Decreasing ureteral stent duration reduces postoperative antibiotic exposure without increasing adverse outcomes in patients undergoing RC. SOURCE OF
Funding: None
