Back
Introduction: Anterior sacrospinous hysteropexy (SSH) was popularized by transvaginal mesh kits. Following market withdrawal, we hypothesized similar efficacy could be achieved through native tissue reattachment of the pubocervical fascia to the cervix with fixation of the anterior cervix to the sacrospinous ligament. Few analyses exist for the efficacy of anterior SSH using native tissue versus mesh augmented repair.
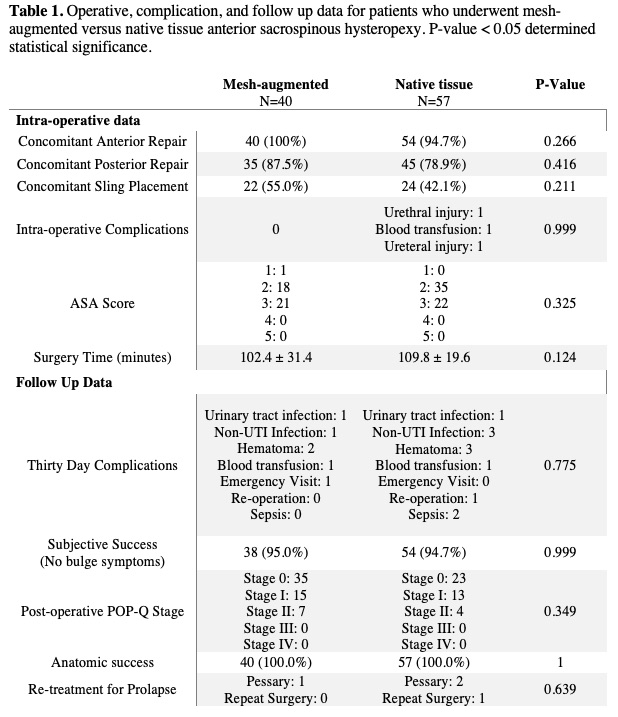
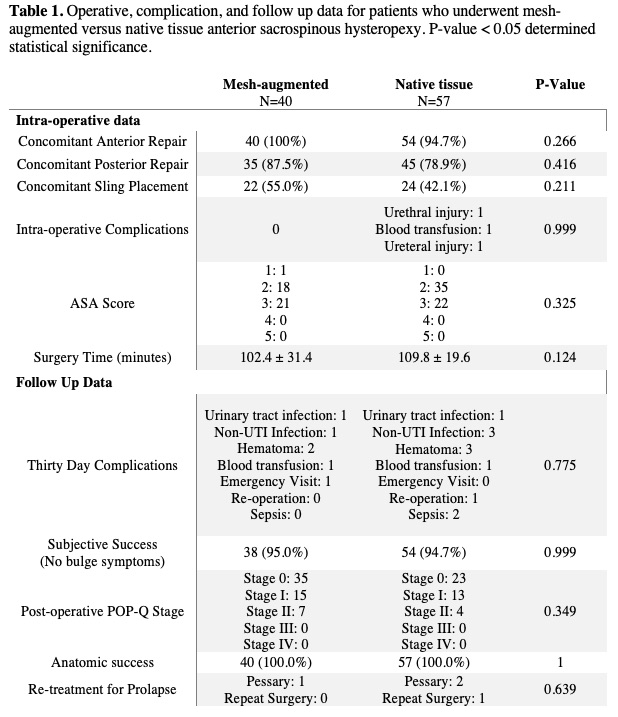
Methods: A retrospective analysis of women who underwent transvaginal SSH at a tertiary center between 01/16-12/21 was performed. Women underwent mesh augmented repair using the Uphold Lite Vaginal Support System or a native tissue anterior SSH. Demographic, clinical, and operative data were reviewed. Composite success was defined as no bulge symptoms, no prolapse retreatment, and no recurrent prolapse beyond the hymen with apex non descended > 1/3 the total vaginal length. Descriptive and bivariate statistics were performed as indicated.
Results: We compared the data for 97 women (40 mesh augmented; 57 native tissue). There was no difference in age, BMI, or vaginal delivery history between groups (p > 0.05). Median pre operative POP Q was stage III. Those in the mesh augmented group were more likely to have undergone a prior prolapse (p=0.003) or intra abdominal (p=0.015) surgery. There was no difference in surgical time (p=0.211) between groups (Table 1). The median post procedure follow up time was 8.2 months. The composite success rate was 95% for all women (Table 1). Anatomic success was demonstrated in 100% of patients. Vaginal bulge symptoms were reported by 2 women in the mesh augmented group compared to 3 in the native tissue group (p=0.999). One woman in the mesh augmented group underwent retreatment (pessary) compared to 3 in the native tissue group (2 pessary, 1 surgery; p=0.639). There was no difference in intra operative (p=0.999) or 30 day post operative (p=0.775) complication rate between groups (Table 1).
Conclusions: Ninety five percent of women who underwent an anterior SSH achieved surgical success. The use of mesh augmentation did not confer any added benefit in terms of efficacy or complications when compared to native tissue. Further long term data is needed to continue our assessment of native tissue anterior SSH. SOURCE OF
Funding: NA
Moderated Poster Session
Session: MP07: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Pelvic Prolapse
MP07-17: Native tissue anterior sacrospinous hysteropexy is an effective and safe approach for primary uterovaginal prolapse compared to mesh augmented repair
Friday, April 28, 2023
9:30 AM – 11:30 AM CST
Location: S401A
- TO
Tyler Lynne Overholt, MD, BS (she/her/hers)
Wake Forest Baptist Health
Poster Presenter(s)
Introduction: Anterior sacrospinous hysteropexy (SSH) was popularized by transvaginal mesh kits. Following market withdrawal, we hypothesized similar efficacy could be achieved through native tissue reattachment of the pubocervical fascia to the cervix with fixation of the anterior cervix to the sacrospinous ligament. Few analyses exist for the efficacy of anterior SSH using native tissue versus mesh augmented repair.
Methods: A retrospective analysis of women who underwent transvaginal SSH at a tertiary center between 01/16-12/21 was performed. Women underwent mesh augmented repair using the Uphold Lite Vaginal Support System or a native tissue anterior SSH. Demographic, clinical, and operative data were reviewed. Composite success was defined as no bulge symptoms, no prolapse retreatment, and no recurrent prolapse beyond the hymen with apex non descended > 1/3 the total vaginal length. Descriptive and bivariate statistics were performed as indicated.
Results: We compared the data for 97 women (40 mesh augmented; 57 native tissue). There was no difference in age, BMI, or vaginal delivery history between groups (p > 0.05). Median pre operative POP Q was stage III. Those in the mesh augmented group were more likely to have undergone a prior prolapse (p=0.003) or intra abdominal (p=0.015) surgery. There was no difference in surgical time (p=0.211) between groups (Table 1). The median post procedure follow up time was 8.2 months. The composite success rate was 95% for all women (Table 1). Anatomic success was demonstrated in 100% of patients. Vaginal bulge symptoms were reported by 2 women in the mesh augmented group compared to 3 in the native tissue group (p=0.999). One woman in the mesh augmented group underwent retreatment (pessary) compared to 3 in the native tissue group (2 pessary, 1 surgery; p=0.639). There was no difference in intra operative (p=0.999) or 30 day post operative (p=0.775) complication rate between groups (Table 1).
Conclusions: Ninety five percent of women who underwent an anterior SSH achieved surgical success. The use of mesh augmentation did not confer any added benefit in terms of efficacy or complications when compared to native tissue. Further long term data is needed to continue our assessment of native tissue anterior SSH. SOURCE OF
Funding: NA