Back
Introduction: Metastatic castration-sensitive prostate cancer (mCSPC) is an incurable disease. Although androgen deprivation therapy (ADT) remains the backbone treatment for patients with mCSPC, multiple randomized studies since 2015 have demonstrated that treatment intensification with the addition of taxanes and/or novel hormonal therapies (NHT) confers significantly improved overall survival. This adds complexity for providers with developing an individual therapeutic approach for patients with mCSPC. Provider prescription patterns for mCSPC are heterogenous, which may present barriers for patients in receiving newer interventions. To investigate this, we conducted a retrospective analysis on the prescription utilization patterns of clinicians initiating treatment for patients with mCSPC.
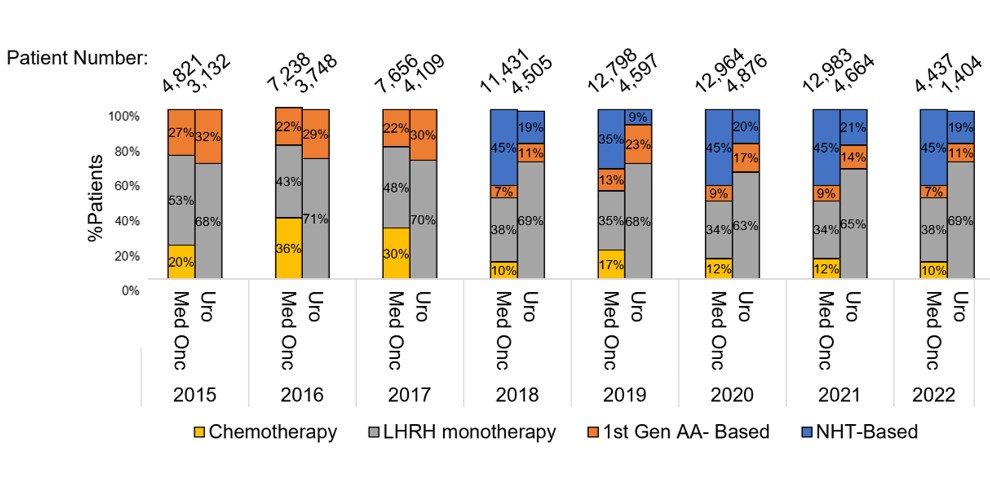
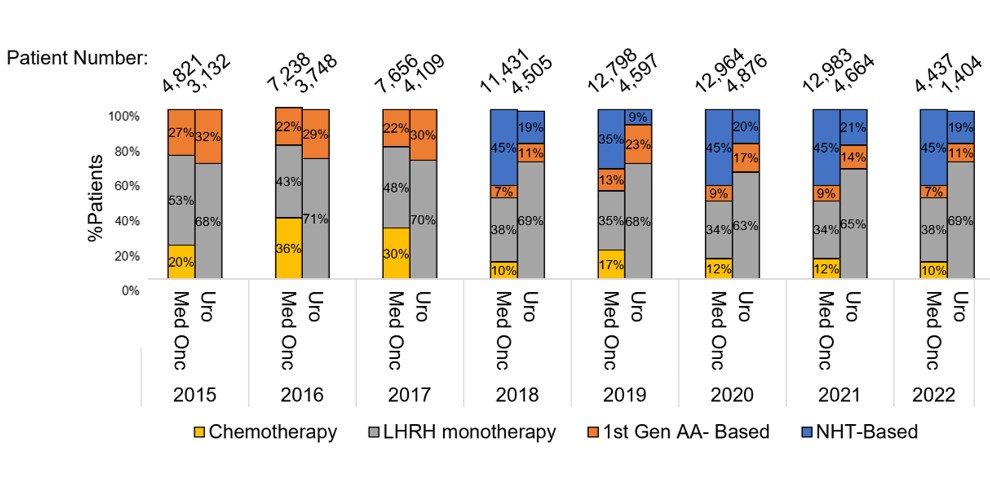
Methods: Pharmacy and claims data were queried from 2015-2022 to identify patients with prostate cancer (PCa). The dataset includes 18 million US cancer patients, including Medicaid, Medicare, Medicare Part D, and cash transactions. Patients with mCSPC were identified using at minimum two ICD9/10 diagnosis codes and/or medications on separate days. Drug classes analyzed include NHT, 1st-generation anti-androgens, chemotherapy, and LHRH monotherapy. Prescription rates of each class of drug were stratified by patient and provider baseline characteristics.
Results: NHT prescription has increased, while chemotherapy, first generation anti-androgens, and LHRH monotherapy have either remained unchanged or decreased since 2015. No variation in prescription patterns were observed between urban and rural settings. Medical oncologists were more likely to prescribe NHT than urologists (45% vs. 19%), whereas urologists were more likely to prescribe LHRH monotherapy (69% v 38%).
Conclusions: Since 2015, NHT utilization and treatment intensification has nationally increased for mCSPC and prescription patterns do not vary between rural and urban settings. When compared to urologists, medical oncologists have more readily incorporated newer therapeutics for mCSPC and decreased the usage of LHRH monotherapy for patients with mCSPC. These data represent a potential area for growth for urologists in the treatment of mCSPC. SOURCE OF
Funding: None
Moderated Poster Session
Session: MP11: Prostate Cancer: Advanced (including Drug Therapy) I
MP11-01: Prescription Patterns of Systemic Therapy in the Management of Metastatic Castration-Sensitive Prostate Cancer
Friday, April 28, 2023
9:30 AM – 11:30 AM CST
Location: S504

Joseph B. Black, MD, PHD
Urology Resident
Beth Israel Deaconess Medical Center
Poster Presenter(s)
Introduction: Metastatic castration-sensitive prostate cancer (mCSPC) is an incurable disease. Although androgen deprivation therapy (ADT) remains the backbone treatment for patients with mCSPC, multiple randomized studies since 2015 have demonstrated that treatment intensification with the addition of taxanes and/or novel hormonal therapies (NHT) confers significantly improved overall survival. This adds complexity for providers with developing an individual therapeutic approach for patients with mCSPC. Provider prescription patterns for mCSPC are heterogenous, which may present barriers for patients in receiving newer interventions. To investigate this, we conducted a retrospective analysis on the prescription utilization patterns of clinicians initiating treatment for patients with mCSPC.
Methods: Pharmacy and claims data were queried from 2015-2022 to identify patients with prostate cancer (PCa). The dataset includes 18 million US cancer patients, including Medicaid, Medicare, Medicare Part D, and cash transactions. Patients with mCSPC were identified using at minimum two ICD9/10 diagnosis codes and/or medications on separate days. Drug classes analyzed include NHT, 1st-generation anti-androgens, chemotherapy, and LHRH monotherapy. Prescription rates of each class of drug were stratified by patient and provider baseline characteristics.
Results: NHT prescription has increased, while chemotherapy, first generation anti-androgens, and LHRH monotherapy have either remained unchanged or decreased since 2015. No variation in prescription patterns were observed between urban and rural settings. Medical oncologists were more likely to prescribe NHT than urologists (45% vs. 19%), whereas urologists were more likely to prescribe LHRH monotherapy (69% v 38%).
Conclusions: Since 2015, NHT utilization and treatment intensification has nationally increased for mCSPC and prescription patterns do not vary between rural and urban settings. When compared to urologists, medical oncologists have more readily incorporated newer therapeutics for mCSPC and decreased the usage of LHRH monotherapy for patients with mCSPC. These data represent a potential area for growth for urologists in the treatment of mCSPC. SOURCE OF
Funding: None