Back
Introduction: A review of children presenting to our emergency department (ED) from 2011 to 2017 found that ureteral stone passage was significantly higher for those prescribed medical expulsive therapy (MET), versus analgesics alone (45% vs 20%, p<0.0001). Urology consultation was also associated with increased MET use (p < 0.0001). As a result, a new nephrolithiasis management protocol was implemented at our ED in August 2017 with the goal of increasing MET usage, decreasing use of CT scans, and increasing outpatient referrals to Urology and Nephrology.
Methods: This is a retrospective study of children aged 2 months to 18 years old who presented to a quaternary children’s hospital ED with an ICD-9 or ICD-10 diagnosis of urolithiasis from August 2017 to April 2022. Basic demographics, MET prescribing, use of CT for stone diagnosis, opioid prescription rate, and referral to Urology and Nephrology were compared before and after implementation of the ED nephrolithiasis protocol. Statistical analysis was performed using two sample t-test analysis and Fisher’s exact test.
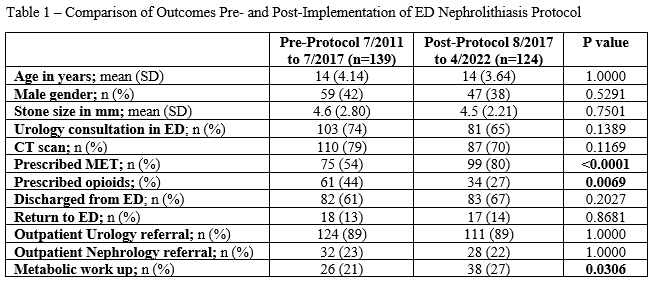
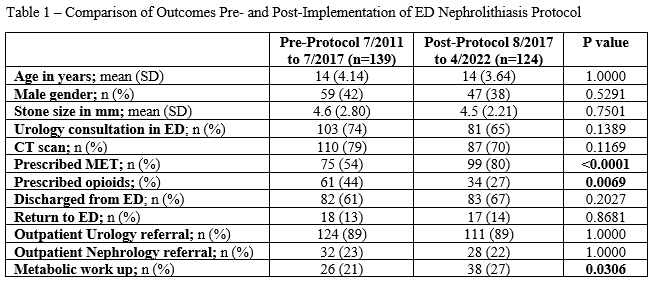
Results: A total of 124 patients met inclusion criteria. Mean age was 14 years (SD 3.64), 47 (38%) male. Comparing pre and post-protocol implementation, there was no difference in mean age, gender, or stone size between groups (Table 1). Post-protocol, 99 patients (80%) were prescribed MET, which was significantly higher compared with 54% prior to the protocol (p < 0.0001). Patients prescribed MET were older (mean 16 vs 15, p=0.014), and a higher proportion were discharged from the ED (71% vs 48%, p=0.033). Post protocol significantly less patients were prescribed opioids (27% vs 44%, p = 0.0069). There was no difference in use of CT scans (79% vs 70%, p = 0.1169), return to the ED (14% vs 14%, p=0.8681), outpatient urology (89% vs 89%, p=1.0) or nephrology referrals (23% vs 22%, p=1.0) pre and post protocol implementation, Table 1.
Conclusions: After implementation of an ED nephrolithiasis protocol, use of MET for ureteral stones increased and prescription of opioids decreased. There was no difference in use of CT scans or outpatient referral to Urology and Nephrology pre versus post-protocol. SOURCE OF
Funding: None
Moderated Poster Session
Session: MP70: Pediatrics V
MP70-17: Implementation of an ED Nephrolithiasis Protocol Increases use of Medical Expulsive Therapy in the Pediatric Population
Monday, May 1, 2023
7:00 AM – 9:00 AM CST
Location: S401A
- DS
Daniel Salevitz, MD, MS (he/him/his)
Mayo Clinic Arizona
Poster Presenter(s)
Introduction: A review of children presenting to our emergency department (ED) from 2011 to 2017 found that ureteral stone passage was significantly higher for those prescribed medical expulsive therapy (MET), versus analgesics alone (45% vs 20%, p<0.0001). Urology consultation was also associated with increased MET use (p < 0.0001). As a result, a new nephrolithiasis management protocol was implemented at our ED in August 2017 with the goal of increasing MET usage, decreasing use of CT scans, and increasing outpatient referrals to Urology and Nephrology.
Methods: This is a retrospective study of children aged 2 months to 18 years old who presented to a quaternary children’s hospital ED with an ICD-9 or ICD-10 diagnosis of urolithiasis from August 2017 to April 2022. Basic demographics, MET prescribing, use of CT for stone diagnosis, opioid prescription rate, and referral to Urology and Nephrology were compared before and after implementation of the ED nephrolithiasis protocol. Statistical analysis was performed using two sample t-test analysis and Fisher’s exact test.
Results: A total of 124 patients met inclusion criteria. Mean age was 14 years (SD 3.64), 47 (38%) male. Comparing pre and post-protocol implementation, there was no difference in mean age, gender, or stone size between groups (Table 1). Post-protocol, 99 patients (80%) were prescribed MET, which was significantly higher compared with 54% prior to the protocol (p < 0.0001). Patients prescribed MET were older (mean 16 vs 15, p=0.014), and a higher proportion were discharged from the ED (71% vs 48%, p=0.033). Post protocol significantly less patients were prescribed opioids (27% vs 44%, p = 0.0069). There was no difference in use of CT scans (79% vs 70%, p = 0.1169), return to the ED (14% vs 14%, p=0.8681), outpatient urology (89% vs 89%, p=1.0) or nephrology referrals (23% vs 22%, p=1.0) pre and post protocol implementation, Table 1.
Conclusions: After implementation of an ED nephrolithiasis protocol, use of MET for ureteral stones increased and prescription of opioids decreased. There was no difference in use of CT scans or outpatient referral to Urology and Nephrology pre versus post-protocol. SOURCE OF
Funding: None