Back
INFECTION/MICROBIOLOGY
Poster Session
(544) Oligomerization mediates mammalian cell toxicity of the human antimicrobial peptide LL-37
Thursday, November 3, 2022
12:00 PM – 12:40 PM ET
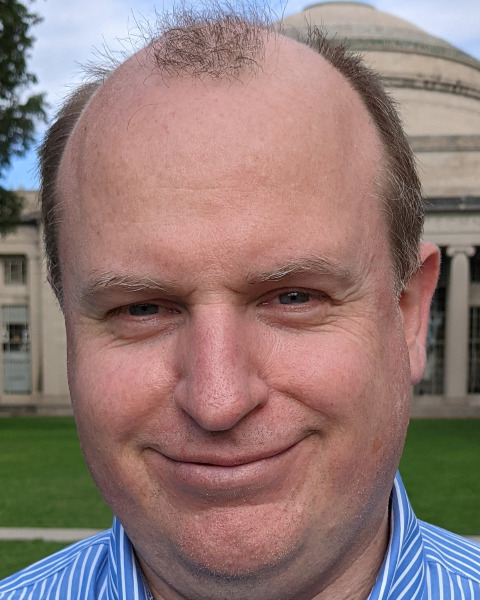
John S. Albin, MD, PhD
Instructor
Massachusetts General Hospital
Cambridge, Massachusetts, United States- BP
Bradley Pentelute, PhD
Professor
Massachusetts Institute of Technology, United States
Presenting Author(s)
Co-Author(s)
Background: Antimicrobial resistance is estimated to have killed almost 1.3 million people in 2019, with that number projected to increase to as much as 10 million per year by 2050[1]. This burden is felt disproportionately by patients with cystic fibrosis, who often carry highly resistant lung pathogens such as Pseudomonas. Although much work has been done in recent decades toward the development of naturally occurring antimicrobial peptides (AMPs) as novel antibiotics for the management of infections with resistant organisms, these efforts have been hampered by a number of technical barriers, not the least of which is excess AMP toxicity. An improved understanding of the mechanisms underlying such toxicity may thus enable the development of nontoxic lead antibiotics based on AMP templates.
Methods: Peptides were synthesized as previously described[2]. Antimicrobial activity was assessed by broth microdilution assays. Hemolytic activity was monitored kinetically by OD600 and as an endpoint measurement by absorbance of free hemoglobin in the supernatant from AMP-treated sheep red blood cells. Biophysical characterization of AMPs consisted of circular dichroism spectroscopy, size exclusion chromatography, and biolayer interferometry.
Results: To better understand the mechanisms underlying mammalian cell toxicity of the human antimicrobial peptide LL-37, we carried out a comprehensive grouped alanine mutagenesis of full-length LL-37, which demonstrated that toxicity maps to C-terminal hydrophobic residues previously implicated in dimerization[3]. Despite loss of hemolytic activity, these derivatives of LL-37 retained both alpha helical structure and antibacterial activity equivalent to that of wild-type LL-37. Further characterization by size exclusion chromatography and biolayer interferometry suggested that loss of toxicity correlated with loss of capacity for self-interaction. Surprisingly, loss of oligomerization appeared to also correlate with inefficient disruption of bacterial membranes. Toward translating this observation to clinical use, we then adapted the mutations associated with loss of hemolytic activity to a novel minimal unit of LL-37, which yielded antibacterial leads with hemolytic activity less than or equal to that of the benchmark therapeutic colistin.
Conclusions: LL-37 hemolytic activity, but not antibacterial activity, correlates with its ability to form multimeric structures. Based on this observation, we have developed antibacterial derivatives of a novel minimal unit of LL-37 that demonstrate toxicity at or below the level of that induced by colistin.
Acknowledgements: Funding for this work includes U19 AI142780 to BLP. Support to JSA includes a Cystic Fibrosis Foundation Shwachman CF Clinical Investigator Award, a prior CFF Postdoctoral Research Fellowship Award, and T32 AI007061.
References: [1] Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet [Internet]. 2022 Feb 12 [cited 2022 Apr 7];399(10325):629–55. Available from: https://www.thelancet.com/article/S0140673621027240/fulltext
[2] Albin JS, Pentelute BL. Efficient flow synthesis of human antimicrobial peptides. Aust J Chem. 2020 Apr 1;73(4):380–8.
[3] Sancho-Vaello E, François P, Bonetti EJ, Lilie H, Finger S, Gil-Ortiz F, et al. Structural remodeling and oligomerization of human cathelicidin on membranes suggest fibril-like structures as active species. Sci Rep. 2017 Dec 1;7(1).
Methods: Peptides were synthesized as previously described[2]. Antimicrobial activity was assessed by broth microdilution assays. Hemolytic activity was monitored kinetically by OD600 and as an endpoint measurement by absorbance of free hemoglobin in the supernatant from AMP-treated sheep red blood cells. Biophysical characterization of AMPs consisted of circular dichroism spectroscopy, size exclusion chromatography, and biolayer interferometry.
Results: To better understand the mechanisms underlying mammalian cell toxicity of the human antimicrobial peptide LL-37, we carried out a comprehensive grouped alanine mutagenesis of full-length LL-37, which demonstrated that toxicity maps to C-terminal hydrophobic residues previously implicated in dimerization[3]. Despite loss of hemolytic activity, these derivatives of LL-37 retained both alpha helical structure and antibacterial activity equivalent to that of wild-type LL-37. Further characterization by size exclusion chromatography and biolayer interferometry suggested that loss of toxicity correlated with loss of capacity for self-interaction. Surprisingly, loss of oligomerization appeared to also correlate with inefficient disruption of bacterial membranes. Toward translating this observation to clinical use, we then adapted the mutations associated with loss of hemolytic activity to a novel minimal unit of LL-37, which yielded antibacterial leads with hemolytic activity less than or equal to that of the benchmark therapeutic colistin.
Conclusions: LL-37 hemolytic activity, but not antibacterial activity, correlates with its ability to form multimeric structures. Based on this observation, we have developed antibacterial derivatives of a novel minimal unit of LL-37 that demonstrate toxicity at or below the level of that induced by colistin.
Acknowledgements: Funding for this work includes U19 AI142780 to BLP. Support to JSA includes a Cystic Fibrosis Foundation Shwachman CF Clinical Investigator Award, a prior CFF Postdoctoral Research Fellowship Award, and T32 AI007061.
References: [1] Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet [Internet]. 2022 Feb 12 [cited 2022 Apr 7];399(10325):629–55. Available from: https://www.thelancet.com/article/S0140673621027240/fulltext
[2] Albin JS, Pentelute BL. Efficient flow synthesis of human antimicrobial peptides. Aust J Chem. 2020 Apr 1;73(4):380–8.
[3] Sancho-Vaello E, François P, Bonetti EJ, Lilie H, Finger S, Gil-Ortiz F, et al. Structural remodeling and oligomerization of human cathelicidin on membranes suggest fibril-like structures as active species. Sci Rep. 2017 Dec 1;7(1).
