Back
Case Series/Study
(CS-005) Case Series: Treatment of Complex Post-Operative Vascular Wounds with a Novel Transforming Powder Dressing (TPD)
Co-Author(s):
Rebecca Barksdale, Registered Nurse; Rajiv Chander, MD; Dian Nesbeth, Nurse Practitioner; Bessie Roca Loor, MD Candidate
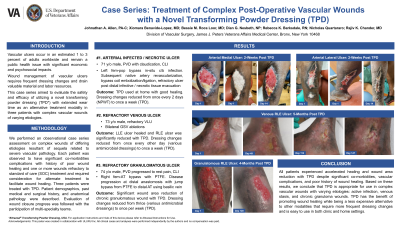
<b>Introduction</b>: <p class="MsoNormal" style="text-align: justify;"><span lang="EN" style="mso-ascii-font-family: Calibri; mso-hansi-font-family: Calibri; mso-bidi-font-family: Calibri; mso-ansi-language: EN;">Vascular ulcers </span><span style="mso-ascii-font-family: Calibri; mso-fareast-font-family: 'Times New Roman'; mso-hansi-font-family: Calibri; mso-bidi-font-family: Calibri;">occur in an estimated 1 to 3 percent of adults worldwide and </span><span lang="EN" style="mso-ansi-language: EN;">remain a public health issue with significant economic and psychosocial impacts. Wound management of vascular ulcers<span style="mso-spacerun: yes;"> </span>require frequent dressing changes and drain valuable material and labor resources. This case series aimed to evaluate </span>the safety and efficacy of utilizing a novel transforming powder dressing (TPD) with extended wear time as an alternative treatment modality in three patients with complex vascular wounds of varying etiologies.</p><br/><br/><b>Methods</b>: <p class="MsoNormal" style="text-align: justify;">We performed an observational case series assessment on complex wounds of differing etiologies resultant of sequela related to severe vascular pathology. Each patient was observed to have vascular complications with history of poor wound healing and significant co-morbidities, were refractory to Standard of Care treatment, and required consideration for alternate treatment to facilitate wound healing. Patient demographics, past medical and surgical history, and anatomical pathology were described. Evaluation of wound closure progress was followed with the participation of multi-specialty teams. Three patients were treated with TPD.</p><br/><br/><b>Results</b>: <p class="MsoNormal" style="margin-bottom: 0in; text-align: justify; line-height: normal; mso-layout-grid-align: none; text-autospace: none;">(1): 71 y/o male with history of PVD, HTN, HLD, substance abuse, s/p popliteal bypass and groin infection. Arteries were revascularized and infective/necrosis was evacuated. Patient continued TPD at home with good healing.</p>
<p class="MsoNormal" style="margin-bottom: 0in; text-align: justify; line-height: normal; mso-layout-grid-align: none; text-autospace: none;"> (2): 73 y/o male with history of HCV, OA, HTN, COPD, stasis dermatitis, bilateral GSV ablations and two refractory ulcerations. LLE ulceration healed and RLE ulceration was significantly reduced with TPD.</p>
<p class="MsoNormal" style="text-align: justify;">(3): 74 y/o male with history of HTN, HIV, PVD progressed to rest pain, tissue loss and refractory shin ulceration after jump bypass for CLI. TPD caused significant wound area reduction <span style="color: black; mso-themecolor: text1;">of the chronic granulomatous wound</span>.</p><br/><br/><b>Discussion</b>: <p class="MsoNormal" style="text-align: justify;">All patients experienced accelerated healing and significant reduction in wound surface area with TPD treatment despite significant co-morbidities, vascular complications, and prior history of poor wound healing. Based on these results, we conclude that TPD is safe and effective for use in a variety of complex vascular wounds with varying etiologies: active infection, venous stasis, and chronic granuloma wounds. TPD has the benefit of promoting wound healing while being a less expensive alternative to other modalities that require more frequent dressing changes and is easy to use in both clinic and home settings. Further large scale studies are warranted.</p><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: <br/><br/>
<p class="MsoNormal" style="margin-bottom: 0in; text-align: justify; line-height: normal; mso-layout-grid-align: none; text-autospace: none;"> (2): 73 y/o male with history of HCV, OA, HTN, COPD, stasis dermatitis, bilateral GSV ablations and two refractory ulcerations. LLE ulceration healed and RLE ulceration was significantly reduced with TPD.</p>
<p class="MsoNormal" style="text-align: justify;">(3): 74 y/o male with history of HTN, HIV, PVD progressed to rest pain, tissue loss and refractory shin ulceration after jump bypass for CLI. TPD caused significant wound area reduction <span style="color: black; mso-themecolor: text1;">of the chronic granulomatous wound</span>.</p><br/><br/><b>Discussion</b>: <p class="MsoNormal" style="text-align: justify;">All patients experienced accelerated healing and significant reduction in wound surface area with TPD treatment despite significant co-morbidities, vascular complications, and prior history of poor wound healing. Based on these results, we conclude that TPD is safe and effective for use in a variety of complex vascular wounds with varying etiologies: active infection, venous stasis, and chronic granuloma wounds. TPD has the benefit of promoting wound healing while being a less expensive alternative to other modalities that require more frequent dressing changes and is easy to use in both clinic and home settings. Further large scale studies are warranted.</p><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: <br/><br/>

.png)