Case Series/Study
(CS-095) A novel approach to sickle cell leg ulcer treatment with the first human keratin graft
Sickle cell leg ulcers (SCLUs) are a painful, recurring, and severe complication of sickle cell disease. Geographical variability exists in the prevalence of SCLUs with the burden ranging from 14% in the United States to as high as 40% in Jamaica [1, 2]. Risk factors for SCLUs encompass demographic characteristics including age > 20 years and male sex as well as patient genotype [3]. The pathophysiology of SCLUs is multifactorial involving nitric oxide deficiency and vascular smooth cell proliferation [4]. This complex pathophysiology contributes to the challenges of comprehensive wound healing in these cases.
Methods:
We present a case of a 40-year-old female with a > 2-month history of right medial ankle SCLU. The patient reported a history of slow healing SCLU with 2 other previous ulcers taking > 6-months to heal. Prior treatment included local wound care, compression therapy, skin substitutes, and split thickness skin grafts. She reported unbearable pain accompanied by infection and the need for antibiotics. Her history was notable for chronic venous insufficiency, iliac vein compression treated with stents, and venous ablation. Vascular assessment revealed no recanalization of the great saphenous vein. She had mild edema but wore compression stockings daily.
Results:
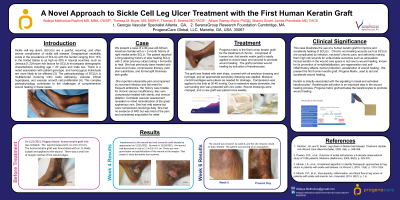
Upon placement of the human keratin graft* the wound measured 1.4 x 2.0 x 0.3 cm. The graft was fenestrated with an 11-blade and applied to the wound. The graft was fixated with steri strips, covered with oil emulsion dressing and hydrogel, and a secondary dressing. Compression was applied. Wound dressings were changed, and a new graft placed weekly.
At week 4, the wound had decreased in size to 1.2 x 0.8 x 0.1 cm. There was new granulation and epithelization of the wound at the margins. The wound resolved completely by week 6, and the site remains closed.
Discussion:
This case illustrates the use of a human keratin graft to improve and accelerate healing of SCLUs.
Trademarked Items: *ProgenaMatrix, ProgenaCare, US.
References: 1. Monfort, J.B. and P. Senet, Leg Ulcers in Sickle-Cell Disease: Treatment Update. Adv Wound Care (New Rochelle), 2020. 9(6): p. 348-356.
2. Powars, D.R., et al., Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicine (Baltimore), 2005. 84(6): p. 363-376.
3. Altman, I.A., et al., A treatment algorithm to identify therapeutic approaches for leg ulcers in patients with sickle cell disease. Int Wound J, 2016. 13(6): p. 1315-1324.
4. Minniti, C.P., et al., Vasculopathy, inflammation, and blood flow in leg ulcers of patients with sickle cell anemia. Am J Hematol, 2014. 89(1): p. 1-6.

.png)