Back
Case Series/Study
(CS-049) Planned Sequential Advanced Treatment Modalities in Diabetic Foot Ulcer Management--A Case report
Co-Author(s):
Katherine Teeters, RN, CWCA,OMS
Introduction: Diabetic foot ulcers often lead to patient morbidity, costs and risk of limb loss. Multiple advanced care modalities have been shown individually to improve wound outcomes, but complete healing remains elusive for many patients. Multiple effective therapies may be used but in an unmethodical manner, leading to prolongation of care, higher costs and longer time for complications . Planned combination sequenced therapies have been useful in a number of disease processes. Using standard principles of wound care, we wish to explore the rational planned sequencing of multiple advanced wound care modalities to optimize wound outcomes and shorten time to healing.
Methods: In order to test a protocol for planned, sequential advanced wound modalities, we initiated the use of negative pressure wound therapy with instillation and dwell, followed by application of a bilayer wound matrix,(silicone and type I collagen matrix) (Theragenesis®) and delayed split thickness skin graft in the treatment of a patient with a Wagner Grade III foot ulcer with osteomyelitis. The case is reported here.
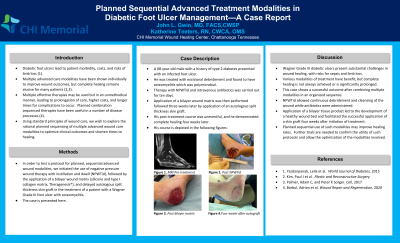
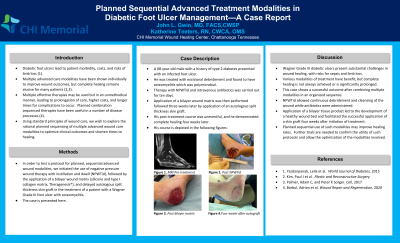
Results: A 68-year-old male with a history of type 2 diabetes presented with an ulcer on his foot. He had a history of a contralateral amputation for a similar problem. He was treated with excisional debridement and found to have osteomyelitis which was polymicrobial. Subsequent therapy with negative pressure wound therapy with instillation and dwell) was carried out for 10 days along with IV antibiotics. He then had application of a bilayer wound matrix (Theragenesis®), and three weeks later had application of an autologous split thickness skin graft. His post-treatment course was uneventful and he demonstrated complete healing four weeks later.
Discussion: Wagner Grade III diabetic ulcers present substantial problems in wound healing, with risks for sepsis and limb loss. Various modalities of treatment have benefit, but complete healing is not always achieved and time to healing is often prolonged This case shows the success of combining multiple modalities in an organized sequence to optimize outcomes. Negative pressure therapy with instillation allowed continuous debridement and cleansing of the wound. Application of a bi-layered tissue product produced a healthy wound bed and facilitated successful application of a skin graft four weeks after initiation of treatment. Planned sequential use of such modalities may improve healing rates and shorten ® time to healing.
Trademarked Items: Theragenesis
References:
Methods: In order to test a protocol for planned, sequential advanced wound modalities, we initiated the use of negative pressure wound therapy with instillation and dwell, followed by application of a bilayer wound matrix,(silicone and type I collagen matrix) (Theragenesis®) and delayed split thickness skin graft in the treatment of a patient with a Wagner Grade III foot ulcer with osteomyelitis. The case is reported here.
Results: A 68-year-old male with a history of type 2 diabetes presented with an ulcer on his foot. He had a history of a contralateral amputation for a similar problem. He was treated with excisional debridement and found to have osteomyelitis which was polymicrobial. Subsequent therapy with negative pressure wound therapy with instillation and dwell) was carried out for 10 days along with IV antibiotics. He then had application of a bilayer wound matrix (Theragenesis®), and three weeks later had application of an autologous split thickness skin graft. His post-treatment course was uneventful and he demonstrated complete healing four weeks later.
Discussion: Wagner Grade III diabetic ulcers present substantial problems in wound healing, with risks for sepsis and limb loss. Various modalities of treatment have benefit, but complete healing is not always achieved and time to healing is often prolonged This case shows the success of combining multiple modalities in an organized sequence to optimize outcomes. Negative pressure therapy with instillation allowed continuous debridement and cleansing of the wound. Application of a bi-layered tissue product produced a healthy wound bed and facilitated successful application of a skin graft four weeks after initiation of treatment. Planned sequential use of such modalities may improve healing rates and shorten ® time to healing.
Trademarked Items: Theragenesis
References:

.png)