Back
Case Series/Study
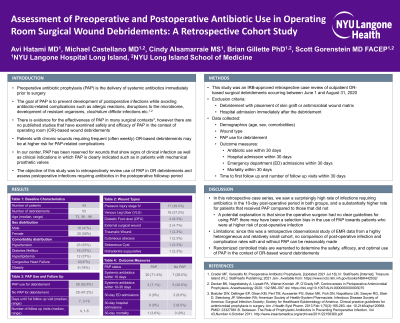
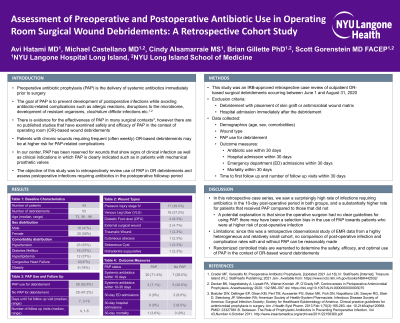
(CS-047) Assessment of Preoperative Antibiotic Prophylaxis in Operating Room Surgical Wound Debridements: A Retrospective Cohort Study
Co-Author(s):
Cindy Alsamarraie, MS – Research Coordinator, Surgery, NYU Langone Health; Michael Castellano, MD – Chief, Division of Wound Care, Surgery, NYU Langone Health; Brian Gillette, PhD – Assistant Professor, Surgery, NYU Langone Health; Avi Hatami, MD – Research Volunteer, Surgery, NYU Langone Health
<b>Introduction</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; mso-themecolor: text1;">Chronic wound-related infections present tremendous health and financial burdens. Surgical debridement reduces risk of infection by removing devitalized tissue and biofilms that inhibit healing. However, the disruption of biofilm during debridement presents risk of bacteria spreading with the potential to cause life- and limb-threatening infections. Preoperative antibiotic prophylaxis (PAP) can prevent development of postoperative infections while avoiding complications of prolonged exposures. While effective PAP protocols exist in many surgical contexts, there are no evidence-based guidelines for PAP in wound debridements. This leaves providers unclear when PAP is indicated and may expose patients to increased risks of infection and antibiotic exposures.</span></p><br/><br/><b>Methods</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; mso-themecolor: text1;">This is an IRB-approved retrospective case review study of patients who underwent operating room surgical </span><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">debridement between June 1- August 31, 2020 <span style="color: black; mso-themecolor: text1;">and October 1 - December 31, 2021</span>. <span style="color: black; mso-themecolor: text1;">Patients were excluded if they were currently on antibiotics at the time of surgery or within 72 hours prior to surgery. All data was collected from Epic EMR System. Patient demographics, wound type, comorbidities, PAP use, and antibiotic prescriptions, signs and symptoms of infection, labs, pathology reports, wound cultures, and emergency department (ED) and hospital admissions were extracted from chart review for descriptive analysis.</span></span></p><br/><br/><b>Results</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black; mso-themecolor: text1;">43 patients with 53 debridements met criteria</span><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">. The population was 58% female with varied etiologies: pressure ulcers (n=17, 39.5%), venous leg ulcers (n=16, 37.2%), diabetic foot ulcers (n=4, 9.3%), and other wound types (n=6, 13.9%). 28 debridements (52.8%) received PAP and 25 (47.2%) did not. Of debridements with PAP, 22 (78.6%) received antibiotics within 30-days; without PAP, 13 (48.0%) received antibiotics within 30-days. Factors associated with antibiotics in follow-up included pain, cellulitis, odor, drainage, positive cultures, and/or </span><a href="https://www.google.com/search?rlz=1C1GCEA_enUS907US907&sxsrf=ALeKk02OaMxSJ-3waaEJlDcP0l9HOUI5Hw:1626360190967&q=osteomyelitis&spell=1&sa=X&ved=2ahUKEwjoitbrp-XxAhVCn-AKHQmAAiMQkeECKAB6BAgBEDA"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: windowtext; text-decoration: none; text-underline: none;">osteomyelitis</span></a><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">. No hospital or ED admissions within 30-days with PAP; one hospital admission, one ED admission, and one ED/hospital admission occurred without PAP.</span></p><br/><br/><b>Discussion</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">It is presumed that PAP can prevent bacteremia during debridement of a colonized/infected wound. Here we saw increased antibiotic use in the 30-day post-op period for patients receiving PAP. One explanation is that there was selection bias. The surgeon had no guidelines for PAP; perhaps it was only ordered for patients with more obvious signs of clinical infection. Because wound patients often receive multiple surgical debridements in a brief period, the judicious use of antibiotics is warranted to decrease any side effects and prevent development of bacterial resistance. A prospective randomized controlled trial assessing the benefit of PAP is warranted.</span></p><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: <br/><br/>

.png)