Back
Clinical Research
(CR-025) Increasing the efficiency of wound assessments with digital technology
Co-Author(s):
Robert Bartlett, MD, CPE, MAPWCA, FAPWH, UHM, FACEP – CMO, Swift Medical; Deborah Babb, PhD, FNP, WOCN – CEO, Valley Wound Healing Center; Robert Fraser, MN, RN – DIRECTOR OF CLINICAL ENGAGEMENT AND EDUCATION, Swift Medical
<b>Introduction</b>: <strong id="docs-internal-guid-b3a147ae-7fff-4be3-fedb-105a3b034d4e" style="font-weight: normal;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">Traditional wound assessment methods are widely used in healthcare settings. However, they can be time-consuming or mismeasure the wound’s surface area because they assume all wounds have rectilinear geometry. Using a wound assessment digital tool improves the standardization of wound assessments and the quality of data collection, while also reducing the time to collect, calculate and document vital wound data. This time-motion study aimed to quantify the time clinicians saved completing wound assessments using a digital tool verses the d<strong id="docs-internal-guid-260a9b98-7fff-7dc3-10ad-da6838da2554" style="font-weight: normal;">ominant </strong>manual methods in a real-world clinical setting. <br /><br /><br /><br /><br /><br /><br /></span></strong><strong id="docs-internal-guid-b3a147ae-7fff-4be3-fedb-105a3b034d4e" style="font-weight: normal;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;"><br /></span></strong><br/><br/><b>Methods</b>: <p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">Four clinicians at an outpatient wound clinic who agreed to join the study were asked to record the time needed to complete wound assessment activities. These activities include capturing wound images, transferring to EMR, measuring and calculating wounds. </span></p>
<strong style="font-weight: normal;"><br /></strong>
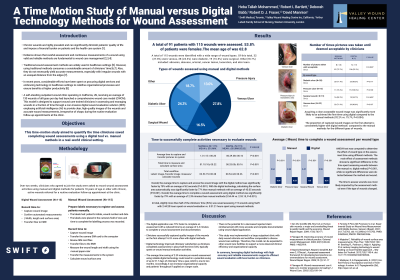
<p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">Over two weeks, clinicians were asked to record these activities using manual and digital methods for patients 18 years of age or older with chronic, active wounds referred for a routine evaluation follow-up appointment at the clinic. A total of 91 patients with 115 wounds were assessed: 27.8% venous ulcers, 24.3% diabetic ulcers, and 16.5% surgical wounds. <br /><br /><br /></span></p><br/><br/><b>Results</b>: <p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">The time to capture and access wound images with the digital technology was significantly faster than manual methods, which relayed on digital cameras and paper rulers. The digital technology was considerably quicker (by 77%) at accurately measuring and calculating the wound surface area (P< 0.001). The overall time to assess wounds was significantly faster by an average of 2.39 minutes using the digital tool. Overall, clinicians completed all steps of the wound assessment using the digital tool in about half of the time (54%) it took them with the manual methods. </span></p>
<p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"> <br /><br /><br /><br /></p><br/><br/><b>Discussion</b>: <strong id="docs-internal-guid-6fa6bd18-7fff-2608-0340-7b6de2ad3ec8" style="font-weight: normal;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">The reduced time to complete wound assessments can be linked to potential cost savings. With an average time savings of two minutes per wound assessment using digital technology, a potential saving of over 50 days of a clinicians’ time is expected a year. Therefore, wound assessment technology would improve clinical throughput and provide extra time to care for patients.<br /><br /><br /><br /><br /></span></strong><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: Ferreira F, Pires IM, Ponciano V, et al. Experimental Study on Wound Area Measurement with Mobile Devices. Sensors (Basel). 2021; 21(17):5762. doi: 10.3390/s21175762. PMID: 34502653; PMCID: PMC8433956.
Majeske C. Reliability of wound surface area measurements. Phys Ther. 1992;72(2):138–41
Bowling FL, Paterson J, Ndip A. Applying 21st century imaging technology to wound healing: an Avant-Gardist approach. J Diabetes Sci Technol. 2013;7(5):1190-4. doi: 10.1177/193229681300700536.<br/><br/>
<strong style="font-weight: normal;"><br /></strong>
<p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">Over two weeks, clinicians were asked to record these activities using manual and digital methods for patients 18 years of age or older with chronic, active wounds referred for a routine evaluation follow-up appointment at the clinic. A total of 91 patients with 115 wounds were assessed: 27.8% venous ulcers, 24.3% diabetic ulcers, and 16.5% surgical wounds. <br /><br /><br /></span></p><br/><br/><b>Results</b>: <p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">The time to capture and access wound images with the digital technology was significantly faster than manual methods, which relayed on digital cameras and paper rulers. The digital technology was considerably quicker (by 77%) at accurately measuring and calculating the wound surface area (P< 0.001). The overall time to assess wounds was significantly faster by an average of 2.39 minutes using the digital tool. Overall, clinicians completed all steps of the wound assessment using the digital tool in about half of the time (54%) it took them with the manual methods. </span></p>
<p dir="ltr" style="line-height: 1.38; margin-top: 0pt; margin-bottom: 0pt;"> <br /><br /><br /><br /></p><br/><br/><b>Discussion</b>: <strong id="docs-internal-guid-6fa6bd18-7fff-2608-0340-7b6de2ad3ec8" style="font-weight: normal;"><span style="font-size: 12pt; font-family: 'Times New Roman'; color: #0e101a; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">The reduced time to complete wound assessments can be linked to potential cost savings. With an average time savings of two minutes per wound assessment using digital technology, a potential saving of over 50 days of a clinicians’ time is expected a year. Therefore, wound assessment technology would improve clinical throughput and provide extra time to care for patients.<br /><br /><br /><br /><br /></span></strong><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: Ferreira F, Pires IM, Ponciano V, et al. Experimental Study on Wound Area Measurement with Mobile Devices. Sensors (Basel). 2021; 21(17):5762. doi: 10.3390/s21175762. PMID: 34502653; PMCID: PMC8433956.
Majeske C. Reliability of wound surface area measurements. Phys Ther. 1992;72(2):138–41
Bowling FL, Paterson J, Ndip A. Applying 21st century imaging technology to wound healing: an Avant-Gardist approach. J Diabetes Sci Technol. 2013;7(5):1190-4. doi: 10.1177/193229681300700536.<br/><br/>

.png)