Case Series/Study
(CS-104) Some said to "chop" but I said "no"
Necrotic heel is known to be the most difficult wound to treat. Most often, this leads to primary amputation even when patient has adequate or palpable pedal pulses. Therefore, it is always advised to avoid attempting limb salvage treatment options. Factors that complicate the healing process for these patients are diabetes, peripheral arterial disease, presence of osteomyelitis in the calcaneus, offloading failure, and history of a previous BKA from the contralateral limb. This case study highlighted the healing success without undergoing partial or total calcanectomy but only utilizing a complex combination of surgical debridement, infection control, and advanced wound medicine.
Methods:
A 56-year-old and well-nourished Caucasian male with PMH of significant uncontrolled type 2 diabetes, status post of the right BKA due to sepsis and infection, and PAD with significant inflow disease of left lower extremity was referred to our clinic from his outside podiatrist who previously treated his necrotic left heel since April 2021. The necrotic heel was healed after using different advanced wound dressings, 6 weeks of oral antibiotics, and incorporation of NPWT and human cellular and tissue-based products (hCTP). Patient was required strictly non-weightbearing using PRAFO boot and wheelchair. Once fully healed, he can transition into CROW boot.
Results:
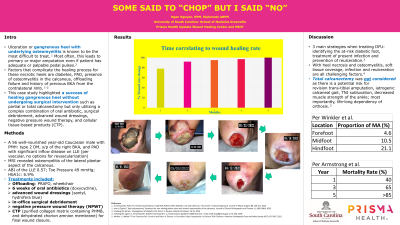
After 6 weeks of oral antibiotics, the osteomyelitis of the calcaneus was adequately controlled. Patient received weekly surgical debridement in the office. After 1 month of weekly in-office surgical debridement, the wound size change was 78.8%. After incorporating negative pressure wound therapy and applications of human cellular and tissue-based products, wound size change was 92% after 3 months, 95% after 4 months and 100% healed after 203 days since the first visit in November 2021. Throughout 203 days of the healing process, patient was completely non-weightbearing and only used PRAFO boot and wheelchair for ambulation. Patient is now in remission.
Discussion:
When treating diabetic foot ulcers, it is important to identify the at-risk diabetic foot, control infection and prevent re-ulceration. With heel necrosis and osteomyelitis, soft tissue coverage is the most challenging factor. It is extremely vital to communicate mortality rates with high-risk patients. Mortality rate increases up to 40% after 1 year, 65% after 3 years and 80% after 5 years making this worse than most malignancies. Partial vs. total calcanectomy was not considered for this specific patient due to a potential risk for revision trans-tibial amputation, iatrogenic calcaneal gait, talonavicular joint subluxation, and decreased muscle strength of the ankle.
Trademarked Items: Puraply AM, Nushield, PRAFO boot, CROW boot,
References:

.png)