Back
Clinical Research
(CR-022) Diabetes Mellitus and its Effect on Lower Extremity Burn Recovery
Co-Author(s):
Elliot Walters, MD – Department of Surgery – University of Texas Medical Branch at Galveston; Alen Palackic, MD – Department of Surgery – University of Texas Medical Branch at Galveston; Steven Wolf, MD – Professor and Chief, Division of Burn and Trauma Surgery, University of Texas Medical Branch at Galveston
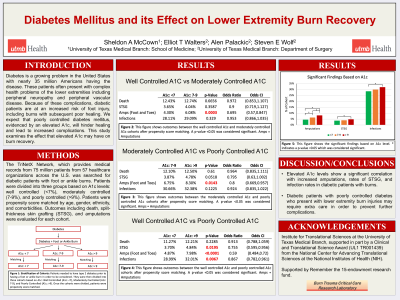
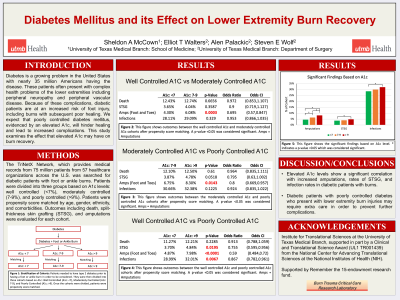
<b>Introduction</b>: <strong id="docs-internal-guid-8ffb6866-7fff-4dc1-c8a7-0a508d306754" style="font-weight: normal;"><span style="font-size: 11pt; font-family: Calibri,sans-serif; color: #000000; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">Diabetes is a growing problem in the United States with nearly 35 million Americans having the disease. These patients often present with complex health problems of the lower extremities including peripheral neuropathy and peripheral vascular disease. Because of these complications, diabetic patients are at an increased risk of foot injuries, including burns, and poor healing. We expect that poorly controlled diabetes mellitus, evidenced by an elevated A1C will hinder healing of burn wounds and lead to increased complications. This study examines the effect that elevated A1C may have on burn recovery.</span></strong><br/><br/><b>Methods</b>: <strong id="docs-internal-guid-b6325ead-7fff-b6d5-aa31-ea7e90e01117" style="font-weight: normal;"><span style="font-size: 11pt; font-family: Calibri,sans-serif; color: #000000; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">The TriNetX Network, which provides medical records from 75 million patients from 57 healthcare organizations across the U.S., was searched for diabetic patients with lower extremity burn injuries. Patients were divided into three groups based on A1C levels: low (< 7%), medium (7-9%), and high ( >9%). Patients were propensity score matched by age, gender, ethnicity, and comorbidities. Outcomes including death, split-thickness skin grafting (STSG), infection, and amputations were evaluated for each cohort.</span></strong><br/><br/><b>Results</b>: <strong id="docs-internal-guid-da7221da-7fff-fd6a-91e9-cc2763e32701" style="font-weight: normal;"><span style="font-size: 11pt; font-family: Calibri,sans-serif; color: #000000; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">When comparing the low A1C and medium A1C groups, there was a significantly increased risk of amputations for the medium A1C group (p=0.0013), and a similar increase in amputations was found for the high A1C group when compared to the medium A1C group (p=0.0086) or low A1C group (p=0.0001). The high A1C group showed an increased incidence of split-thickness skin grafting (p=0.045) as well as infection rates (p=0.0067) when compared to the low A1C group. There was no significant difference in mortality between any of the A1C cohorts.</span></strong><br/><br/><b>Discussion</b>: <strong id="docs-internal-guid-99bf1961-7fff-910f-a85d-a6065701cd56" style="font-weight: normal;"><span style="font-size: 11pt; font-family: Calibri,sans-serif; color: #000000; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">Elevated A1C levels show a significant correlation with increased amputations in diabetic patients with burns. This points to the importance of effective glycemic control in the pre-injury setting. Further investigation is needed on interventions to reduce limb loss in injured patients with poorly controlled hyperglycemia.</span></strong><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: <br/><br/>

.png)