Case Series/Study
(CS-022) Use of Applied Keratin Matrix Over An Operative Site To Accelerate Incisional Healing Rate in Diabetic Patients
Keratin has recently been studied for its potential to accelerate healing in wounds due to its effect on fibroblasts and keratinocytes. Fibroblasts play a key role in early wound healing and human keratin has been associated with increased fibroblast attachment and proliferation both vital to coaptation of a surgical incision. Keratinocytes are active in later stages of wound healing with applied keratin demonstrating an increase in keratinocyte activation leading to increased epithelialization of a wound.
Incision healing times vary depending on type of and location of surgery but there are generally accepted rates reported. Patients with comorbid conditions such as diabetes, peripheral vascular disease, auto-immune disease, renal disease and heart disease have been documented to potentially demonstrate slow or complicated healing. Delayed healing of post-operative incisions is purported to lead to increase potential for post-operative infection, increased scarring, and potential decrease in wound strength.
The purpose of this study is to evaluate the effect of keratin matrix applied topically over an incision to potentially increase healing rate and reduce scarring of a surgical incision in difficult to heal diabetic patients.
Methods:
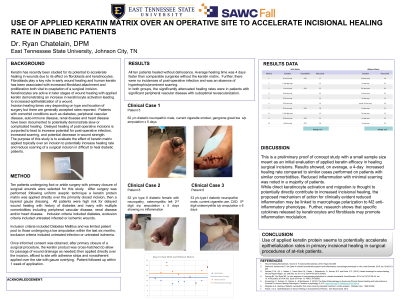
Ten patients undergoing foot or ankle surgery with primary closure of surgical wounds were selected for this study. After surgery was performed following uniform aseptic technique a keratin protein matrix was applied directly over the primarily closed incision, then a layered gauze dressing. All patients were high risk for delayed wound healing with history of diabetes and many with multiple comorbidities including peripheral vascular disease, renal disease and/or heart disease. Inclusion criteria included diabetes, exclusion criteria included untreated infected or ischemic wounds.
Results:
All ten patients healed without dehiscence with healing rate comparable to nondiabetics and in some cases healing faster than typical nondiabetic rate. Further, there were no incidences of post-operative infection with absence of hypertrophic/prominent scarring.
Discussion:
This is a preliminary study with a small sample size and meant as an initial evaluation of applied keratin efficacy in healing surgical incisions. Initial results showed an at least similar if not increased healing rate of diabetic to non-diabetic patients, and minimal scarring was noted in patients.
Trademarked Items:
References: Pastar, I et al. Epithelialization in Wound Healing: A Comprehensive Review. Adv Wound Care, 2014.
Pechter, P. M., Gil, J., Valdes, J., Tomic-Canic, M., Pastar, I., Stojadinovic, O., Kirsner, R.S. and Davis, S.C. (2012), Keratin dressings for wound healing. Wound Repair Regen, 20: 236-242. doi:10.1111/j.1524-475X.2012.00768.x
Russo B, Brembilla NC, Chizzolini C. Interplay Between Keratinocytes and Fibroblasts: A Systematic Review Providing a New Angle for Understanding Skin Fibrotic Disorders. Front Immunol. 2020 May 6;11:648. doi: 10.3389/fimmu.2020.00648. PMID: 32477322; PMCID: PMC7232541.
Wang S, Taraballi F, Tan LP, Ng KW. Human keratin hydrogels support fibroblast attachment and proliferation in vitro. Cell Tissue Res. 2012 Mar;347(3):795-802. doi: 10.1007/s00441-011-1295-2. PMID: 22287039.
Waters M, Vandevorde P, Van Dyke M. Keratin biomaterials augment anti-inflammatory macrophage phenotyple in vitro. Acta Biomater. 2018 Jan 15;66:213-223
Werner S, Krieg T, Smola H. Keratinocyte-fibroblast interactions in wound healing. J Invest Dermatol. 2007 May;127(5):998-1008. doi: 10.1038/sj.jid.5700786. PMID: 17435785.
Wound Healing Biomaterials, Volume 2: Functional Biomaterials, 2016, Pages 353-365

.png)