Case Series/Study
(CS-092) Comparable clinical effects of the autologous combined leucocyte, platelet and fibrin on diabetic foot ulcers despite very low ABI values in the affected limb.
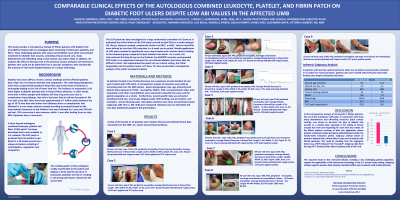
This study provide an analysis of fifteen patients treated with an autologous patch consisting of fibrin, leukocytes and platelets. These patients have failed conventional treatment for diabetic foot wounds, consisting of local wound care, sharp debridement and offloading using a total contact cast system.
Methods: The autologous combined leucocyte, platelet, and fibrin patch, is a novel treatment created by a unique centrifugation of autologous blood is known to contain growth factors key for angiogenesis. The patch is applied to chronic diabetic foot wounds that have failed conventional wound care treatment alone.
Results: Fifteen patients have failed at least four weeks of conventional wound care (average 16 weeks). These patients continued to have a wound size of more than fifty percent of their original size at four weeks, despite weekly sharp debridement, local wound care and total contact cast offloading. All patients presented with type II diabetes, peripheral arterial disease (diagnosed as having a peripheral vascular procedure within one year and/or on conventional anticoagulation medication). Four patients were on hemodialysis. The patch was applied weekly, one to twenty applications (mean 7.5 applications) per patient were done. Patient age range was 37-89 years old (mean 59). In this patient population, after one application of a patch, in conjunction with sharp debridement, local wound care and adjunctive total contact casting, the average decrease in length was 22.5%, width decrease was 16.45%, depth decrease was 4.5% and total surface area decrease was 20.25%. Healing rates and time to healing were compared between groups with ABI >0.8 and ABI < 0.8. Comparable healing rates were seen in the two populations.
Discussion:
In our case series of fifteen patients, the use of the autologous patch, in conjunction with sharp debridement and offloading measures, has shown to decrease the size of diabetic foot wounds on a weekly basis, even in more ischemic limbs. Of the fifteen patients evaluated, eleven patients completely healed (complete epithelialization) with the use of the patch during the twenty week evaluation period. One patient underwent a minor (hallux) amputation. Three patients have continued care with noted improvement in their wound on a weekly basis.
Trademarked Items:
References:

.png)