Case Series/Study
(CS-006) Antiphospholipid Syndrome Skin Ulcerations Improved With Change Of Anticoagulation Treatment
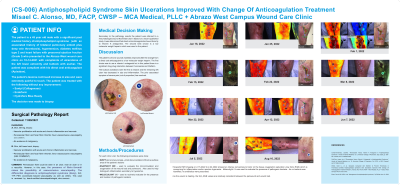
The patient is a 45 year old male with a significant past medical history of antiphospholipid syndrome with a history of bilateral pulmonary emboli with deep vein thrombosis, hypertension, diabetes mellitus type 2 and heart failure with preserved ejection fraction (Grade I) who presented to the Abrazo West wound care clinic on 10-14-2021 with complaints of ulcerations of the left lower extremity calf and buttock with formation of eschar.
The patient has remained compliant with his direct oral anticoagulant (Apixaban), but the ulcers gradually worsened with the appearance of Livedo reticularis/ Livedo racemose. Associated symptoms include pain out of proportion with skin necrosis.
The decision was made to perform punch biopsies as the lesions continued to worsen despite treatment with:
< ![if !supportLists] >· < ![endif] >Collagenase enzymatic debridement
< ![if !supportLists] >· < ![endif] >Selective debridements
< ![if !supportLists] >· < ![endif] >Application of collagens and antimicrobial secondary dressings
The pathology report from skin biopsies:
11-9-2021
DIAGNOSIS:
A. Skin, left leg, biopsy:
- Vascular proliferation with acute and chronic inflammation and necrosis.
- Perivascular fibrin and focal fibrin thrombi; favor vaso-occlusive vasculopathy
- No evidence of malignancy.
B. Skin, left lower back, biopsy:
- Vascular proliferation with acute and chronic inflammation and necrosis.
- Perivascular fibrin and focal fibrin thrombi; favor vaso-occlusive vasculopathy
- No evidence of malignancy.
COMMENT:
Perivascular fibrin could be seen in an ulcer, near an ulcer or in a vasculitis. However, in this case, the presence of fibrin thrombi raises the possibility of vaso-occlusive vasculopathy. The differential diagnosis is antiphospholipid syndrome (likely)
Methods:
Snapshot NIR used to evaluate the microcirculation and oxygenation of lesions in addition to inflammation.
Moleculight i:X used to evaluate for the presence of pathogenic bacteria
Referral to Rheumatology done after the pathology report
Recommendation made to discontinue direct oral anticoagulation with Apixaban in favor of Enoxaparin. Coumadin was not used secondary to potential drug to drug interaction with Fluconazole
Results:
The patient’s vasculitic wounds began improving and healing after changing from direct oral anticoagulation with Apixaban to Enoxaparin.
Discussion:
DISCUSSION
Recent studies have now shown superiority of treating antiphospholipid syndrome with Coumadin or Enoxaparin therapy. Direct oral anticoagulation is no longer recommended for treatment of antiphospholipid syndrome
Trademarked Items: SNAPSHOT NIR
MOLECULIGHT I:X
SWIFT SKIN AND WOUND APP
References: UpToDate
Management of antiphospholipid syndrome
Authors:Doruk Erkan, MD, MPHThomas L Ortel, MD, PhDSection Editor:David S Pisetsky, MD, PhDDeputy Editors:Monica Ramirez Curtis, MD, MPHJennifer S Tirnauer, MD
Contributor Disclosures
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: May 2022. | This topic last updated: Dec 14, 2021.

.png)