Case Series/Study
(CS-125) Fish skin is a superior acellular dermal matrix for the treatment of pilonidal cyst
Pilonidal cysts (PCs), cysts that develop in the sacrococcygeal region, are common and frequently impact healthy young males. PCs are associated with increased morbidity, decreased quality of life, embarrassment, and, if untreated, an increased risk of squamous cell carcinoma1. The etiology and risk factors have previously been reported, with location, gender, ethnicity, and the presence of anaerobic bacteria in hair follicles being consistent. Conservative treatment options range from phenol injections, simple excision and drainage, excision and unroofing with healing from secondary intention, and excision and drainage with primary closure1. In more advanced cases, reconstructive skin flaps are utilized1. Comparatively, conservative methodologies are economically responsible if successful and require less invasive techniques. Advanced adjunctive biologics bridge flap revisions and expedite tissue regeneration during primary or secondary wound healing following excision and drainage. Fish skin graft (FSG) is a relatively new and promising matrix with the versatility to manage varying clinical treatment goals. FSG is minimally processed, has the utility to augment cell migration and neovascularization, and is rich in Omega3 fatty acids shown to be bacteriostatic2,3,4.
Methods:
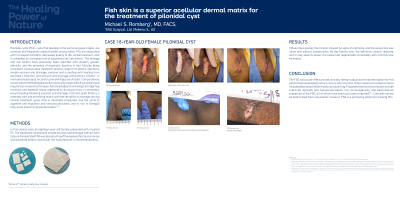
In this clinical case, an eighteen-year-old female presented with a typical PC. The treatment consisted of simple excision and drainage with primary closure. Fenestrated FSG was placed on top of the exposed fascia as an onlay and bolstered before closure per the manufacturer’s recommendations.
Results:
Fifteen days postop, the incision showed no signs of erythema, and the suture line was intact and without complication. By day twenty-nine, the definitive closure resolved, and on day seventy-seven, the tissue had regenerated remarkably with minimal scar formation.
Discussion:
The FSG was a cost-effective and clinically relevant adjunctive treatment option for this patient that expediated primary closure after excision. Other noted clinical observations included decreased inflammation and scarring. Proposed mechanisms of action include rapid cell ingrowth and neovascularization, low immunogenicity, and bacteriostatic properties of the FSG, all of which have previously been reported2,3,4. Causality cannot be determined from one patient; however, FSG is a promising option for treating PCs.
Trademarked Items: *KerecisTM, Kerecis, Isafjordur, Iceland
References: 1. Kober MM, Alapati U, Khachemoune A. Treatment options for pilonidal sinus. Cutis. 2018 Oct;102(4):E23-E29. PMID: 30489572.
2. Magnusson S, Baldursson BT, Kjartansson H, Rolfsson O, Sigurjonsson GF. Regenerative and Antibacterial Properties of Acellular Fish Skin Grafts and Human Amnion/Chorion Membrane: Implications for Tissue Preservation in Combat Casualty Care. Mil Med. 2017 Mar;182(S1):383-388. doi: 10.7205/MILMED-D-16-00142. PMID: 28291503.
3. Stone R 2nd, Saathoff EC, Larson DA, Wall JT, Wienandt NA, Magnusson S, Kjartansson H, Natesan S, Christy RJ. Accelerated Wound Closure of Deep Partial Thickness Burns with Acellular Fish Skin Graft. Int J Mol Sci. 2021 Feb 4;22(4):1590. doi: 10.3390/ijms22041590. PMID: 33557424; PMCID: PMC7915828.
4. Baldursson BT, Kjartansson H, Konrádsdóttir F, Gudnason P, Sigurjonsson GF, Lund SH. Healing rate and autoimmune safety of full-thickness wounds treated with fish skin acellular dermal matrix versus porcine small-intestine submucosa: a noninferiority study. Int J Low Extrem Wounds. 2015 Mar;14(1):37-43. doi: 10.1177/1534734615573661. Epub 2015 Mar 9. PMID: 25759413.

.png)