Back
Case Series/Study
(CS-033) The Impossible Solution: Pure Hypochlorous Acid Preserved Cleanser with and without NPWT for Secondary Healing in a Complex Abdominal Wound with Fistula
Co-Author(s):
Krista Bauer, RN, WCC, OMS; Kari Day, RN, BSN, WCC; Ashley Wardman, CPPM, Surgical LPN-C
<b>Introduction</b>: <p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">The use of pure Hypochlorous Acid (HOCl) in wound preparation is well accepted. Recent guidelines suggest HOCL cleansers can mechanically remove necrotic debris and microbial matter from the wounds safely.</span></p>
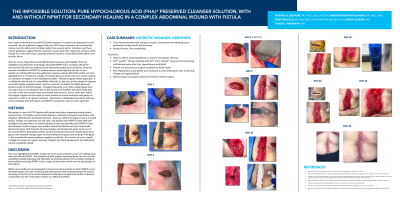
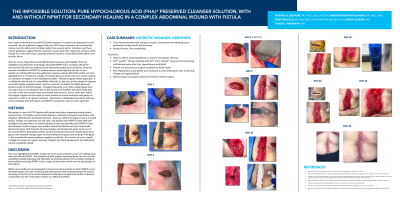
<p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">The use of pure Hypochlorous Acid (pHA) with Negative Pressure instillation technology with dwell (NPWTi-d) is emergent. We prefer this method with pHA in preparation for surgical closure. However, wounds unsuitable for NPWT benefit from gauze soaked with HOCl solution or pHA application for 5-10 minutes soaking. Moistened gauze is a traditional method and its simplicity supports such use. We present a challenging case where pHA solution was used effectively with both gauze and NPWTi-d. </span></p><br/><br/><b>Methods</b>: <p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">We present a challenging case of a 33 YO woman with a bowel perforation following a robotic hysterectomy.<span style="mso-spacerun: yes;"> </span>The highly contaminated abdomen underwent emergent exploration with irrigation, debridement, and bowel resection. HOCL with pHA was utilized throughout a 6-month period.<span style="mso-spacerun: yes;"> </span>Initially, the abdomen was left open and treated with NPWTi-d with pHA. An enterocutaneous fistula was identified and NPWTi-d was discontinued. Further surgery was avoided and the wound bed with fistula was then treated with pHA/moistened gauze. Patient was discharged to home, and the wound treated with pHA moistened gauze, with an ostomy appliance over the actively draining fistula. At 6 months, the drainage stopped, the fistula closed, and the abdominal wound completely healed. </span></p><br/><br/><b>Results</b>: <p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">Pure Hypochlorous Acid (HOCl) can be beneficial both with and without NPWT and may be particularly useful in the treatment of an abdominal wound with fistula.</span></p><br/><br/><b>Discussion</b>: <span style="font-size: 11.0pt; line-height: 107%; font-family: 'Calibri',sans-serif; mso-ascii-theme-font: minor-latin; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-hansi-theme-font: minor-latin; mso-bidi-font-family: 'Times New Roman'; mso-bidi-theme-font: minor-bidi; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">This case highlights the benefits of pHA in the acute and post-acute care settings both with and without NPWT. The simplicity of pHA soaked moistened gauze successfully expedited hospital discharge and ultimately successfully allowed for secondary healing without resuming NPWT and/or surgical intervention.<span style="mso-spacerun: yes;"> </span><span style="mso-spacerun: yes;"> </span></span><br/><br/><b>Trademarked Items</b>: *Vashe: Wound Solution
* (Urgo Medical)<br/><br/><b>References</b>: REFERENCES
1. Robson MC, History of hypochlorous acid and its mechanism of action. Supplement to Wounds 2019; S46-48.
2. Robson MC, Disruption of biofilm with Vashe wound solution History of hypochlorous acid and its mechanism of action. Supplement to Wounds 2019; S59-60
3. Tran BNN, Chen AD, Kamali P, Singhal D., Lee BT, and Fukudome EY. National perioperative outcomes of flap coverage for pressure ulcers from 2005 to 2015 using American College of Surgeons National Surgical Quality Improvement Program. Archives of plastic surgery 2018 45(5), 418.
4. Kim PJ, Attinger CE, Cjstantine, T. et al. Negative pressure wound therapy with instillation: International consensus guidelines update. Int Wound J. 2019;1-13<br/><br/>
<p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">The use of pure Hypochlorous Acid (pHA) with Negative Pressure instillation technology with dwell (NPWTi-d) is emergent. We prefer this method with pHA in preparation for surgical closure. However, wounds unsuitable for NPWT benefit from gauze soaked with HOCl solution or pHA application for 5-10 minutes soaking. Moistened gauze is a traditional method and its simplicity supports such use. We present a challenging case where pHA solution was used effectively with both gauze and NPWTi-d. </span></p><br/><br/><b>Methods</b>: <p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">We present a challenging case of a 33 YO woman with a bowel perforation following a robotic hysterectomy.<span style="mso-spacerun: yes;"> </span>The highly contaminated abdomen underwent emergent exploration with irrigation, debridement, and bowel resection. HOCL with pHA was utilized throughout a 6-month period.<span style="mso-spacerun: yes;"> </span>Initially, the abdomen was left open and treated with NPWTi-d with pHA. An enterocutaneous fistula was identified and NPWTi-d was discontinued. Further surgery was avoided and the wound bed with fistula was then treated with pHA/moistened gauze. Patient was discharged to home, and the wound treated with pHA moistened gauze, with an ostomy appliance over the actively draining fistula. At 6 months, the drainage stopped, the fistula closed, and the abdominal wound completely healed. </span></p><br/><br/><b>Results</b>: <p class="yiv7405506440msonormal" style="background: white;"><span style="color: black; mso-color-alt: windowtext;">Pure Hypochlorous Acid (HOCl) can be beneficial both with and without NPWT and may be particularly useful in the treatment of an abdominal wound with fistula.</span></p><br/><br/><b>Discussion</b>: <span style="font-size: 11.0pt; line-height: 107%; font-family: 'Calibri',sans-serif; mso-ascii-theme-font: minor-latin; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-hansi-theme-font: minor-latin; mso-bidi-font-family: 'Times New Roman'; mso-bidi-theme-font: minor-bidi; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">This case highlights the benefits of pHA in the acute and post-acute care settings both with and without NPWT. The simplicity of pHA soaked moistened gauze successfully expedited hospital discharge and ultimately successfully allowed for secondary healing without resuming NPWT and/or surgical intervention.<span style="mso-spacerun: yes;"> </span><span style="mso-spacerun: yes;"> </span></span><br/><br/><b>Trademarked Items</b>: *Vashe: Wound Solution
* (Urgo Medical)<br/><br/><b>References</b>: REFERENCES
1. Robson MC, History of hypochlorous acid and its mechanism of action. Supplement to Wounds 2019; S46-48.
2. Robson MC, Disruption of biofilm with Vashe wound solution History of hypochlorous acid and its mechanism of action. Supplement to Wounds 2019; S59-60
3. Tran BNN, Chen AD, Kamali P, Singhal D., Lee BT, and Fukudome EY. National perioperative outcomes of flap coverage for pressure ulcers from 2005 to 2015 using American College of Surgeons National Surgical Quality Improvement Program. Archives of plastic surgery 2018 45(5), 418.
4. Kim PJ, Attinger CE, Cjstantine, T. et al. Negative pressure wound therapy with instillation: International consensus guidelines update. Int Wound J. 2019;1-13<br/><br/>

.png)