Back
Case Series/Study
(CS-034) The Use of Aseptically Processed Meshed Reticular Acellular Dermal Matrix in Soft Tissue Necrotizing Infection
Co-Author(s):
Krista Bauer, ), RN, WCC, OMS,; Kari Day, RN, BSN, WCC; Ashley Wardman, CPPM, Surgical LPN-C
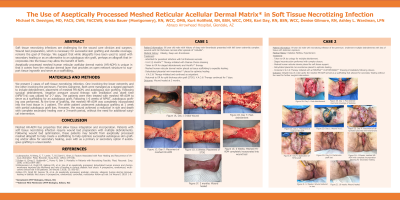
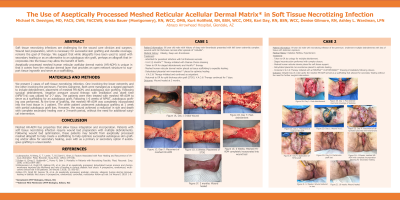
<b>Introduction</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif;">Soft tissue necrotizing infections are challenging for the wound care clinician and surgeon. Wound bed preparation, which is necessary for successful skin grafting and durable coverage, remains the goal of therapy.<span style="mso-spacerun: yes;"> </span>We suggest that while allografts have been used to assist with secondary healing or as an alternative to an autologous skin graft, perhaps an allograft that incorporates into the tissue may allow the benefit of both.</span></p>
<p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif;">Aseptically processed meshed human reticular acellular dermal matrix (HR-ADM) is unique in that it comes from the reticular dermal layer that provides an open network structure to support tissue ingrowth and serve as a scaffolding.</span></p><br/><br/><b>Methods</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif;">We present 2 cases of soft tissue necrotizing infection.<span style="mso-spacerun: yes;"> </span>One involving the lower extremity and the other involving the perineum, Forniers Gangrene. Both were managed as a staged approach to include debridement, placement of meshed HR-ADM, and autologous skin grafting. Following surgical debridement, negative pressure wound therapy with instillation and dwell time (NPWTi d*) was utilized for 2-7 days. <span style="mso-spacerun: yes;"> </span>The patients were then treated with meshed HR-ADM to serve as a scaffolding for an autologous graft.<span style="mso-spacerun: yes;"> </span>Following 1-6 weeks of NPWT, autologous grafting was performed.<span style="mso-spacerun: yes;"> </span>At the time of grafting, the meshed HR-ADM was completely incorporated into the host tissue in 1 patient.<span style="mso-spacerun: yes;"> </span>The other patient underwent autologous grafting at 1 week with partial autologous graft loss.<span style="mso-spacerun: yes;"> </span>However, the wound achieved a reduction in size and depth with complete secondary healing over a 3-month period, without the need for additional surgical intervention.</span></p><br/><br/><b>Results</b>: Aseptically processed meshed allograft can help create a scaffolding to help optimize successful autologous skin grafting and or allow for secondary healing in patients with necrotizing infection.<br/><br/><b>Discussion</b>: <span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Meshed HR-ADM has properties that allow tissue integration and incorporation. Patients with soft tissue necrotizing infection require wound bed preparation with multiple debridements.<span style="mso-spacerun: yes;"> </span>Following wound bed optimization, these patients may benefit from aseptically processed meshed allograft to help create a scaffolding to help optimize successful autologous skin grafting and or allow for secondary healing, event with as a primary or secondary option if autologous grafting is unsuccessful.</span><br/><br/><b>Trademarked Items</b>: *SomaGen (Human Reticular Dermal Matrix)
(MTF Biologics)<br/><br/><b>References</b>: REFERENCES
1. Labropoulos, N Wang, E, T. Lanier, T, B.S.Sami U. Khan,U, Factors Associated with Poor Healing and Recurrence of Venous Ulceration Plast. Reconstr. Surg 2012; 129(1):179-186.
2. Golger A, Ching S, Goldsmith C, Penny R, Bain J: Mortality in Patients with Necrotizing Fasciitis. Plast. Reconstr. Surg 2006; 119(6):1804-1807.
3. DiDomenico LA, Orgill DP, Galiano RD, et al. Use of an aseptically processed, dehydrated human amnion and chorion membrane improves the likelihood and rate of healing in chronic diabetic foot ulcers: A prospective, randomized, multi-centre clinical trial in 80 patients. Int Wound J 2018; 15: 950-957.
4. Zelen CM, Orgill DP, Serena TE, et al. An aseptically processed, acellular, reticular, allogenic human dermis improves healing in diabetic foot ulcers: A prospective, randomized, controlled, multicenter follow-up trial. Int Wound J 2018: 1-9.<br/><br/>
<p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif;">Aseptically processed meshed human reticular acellular dermal matrix (HR-ADM) is unique in that it comes from the reticular dermal layer that provides an open network structure to support tissue ingrowth and serve as a scaffolding.</span></p><br/><br/><b>Methods</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif;">We present 2 cases of soft tissue necrotizing infection.<span style="mso-spacerun: yes;"> </span>One involving the lower extremity and the other involving the perineum, Forniers Gangrene. Both were managed as a staged approach to include debridement, placement of meshed HR-ADM, and autologous skin grafting. Following surgical debridement, negative pressure wound therapy with instillation and dwell time (NPWTi d*) was utilized for 2-7 days. <span style="mso-spacerun: yes;"> </span>The patients were then treated with meshed HR-ADM to serve as a scaffolding for an autologous graft.<span style="mso-spacerun: yes;"> </span>Following 1-6 weeks of NPWT, autologous grafting was performed.<span style="mso-spacerun: yes;"> </span>At the time of grafting, the meshed HR-ADM was completely incorporated into the host tissue in 1 patient.<span style="mso-spacerun: yes;"> </span>The other patient underwent autologous grafting at 1 week with partial autologous graft loss.<span style="mso-spacerun: yes;"> </span>However, the wound achieved a reduction in size and depth with complete secondary healing over a 3-month period, without the need for additional surgical intervention.</span></p><br/><br/><b>Results</b>: Aseptically processed meshed allograft can help create a scaffolding to help optimize successful autologous skin grafting and or allow for secondary healing in patients with necrotizing infection.<br/><br/><b>Discussion</b>: <span style="font-size: 12.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Meshed HR-ADM has properties that allow tissue integration and incorporation. Patients with soft tissue necrotizing infection require wound bed preparation with multiple debridements.<span style="mso-spacerun: yes;"> </span>Following wound bed optimization, these patients may benefit from aseptically processed meshed allograft to help create a scaffolding to help optimize successful autologous skin grafting and or allow for secondary healing, event with as a primary or secondary option if autologous grafting is unsuccessful.</span><br/><br/><b>Trademarked Items</b>: *SomaGen (Human Reticular Dermal Matrix)
(MTF Biologics)<br/><br/><b>References</b>: REFERENCES
1. Labropoulos, N Wang, E, T. Lanier, T, B.S.Sami U. Khan,U, Factors Associated with Poor Healing and Recurrence of Venous Ulceration Plast. Reconstr. Surg 2012; 129(1):179-186.
2. Golger A, Ching S, Goldsmith C, Penny R, Bain J: Mortality in Patients with Necrotizing Fasciitis. Plast. Reconstr. Surg 2006; 119(6):1804-1807.
3. DiDomenico LA, Orgill DP, Galiano RD, et al. Use of an aseptically processed, dehydrated human amnion and chorion membrane improves the likelihood and rate of healing in chronic diabetic foot ulcers: A prospective, randomized, multi-centre clinical trial in 80 patients. Int Wound J 2018; 15: 950-957.
4. Zelen CM, Orgill DP, Serena TE, et al. An aseptically processed, acellular, reticular, allogenic human dermis improves healing in diabetic foot ulcers: A prospective, randomized, controlled, multicenter follow-up trial. Int Wound J 2018: 1-9.<br/><br/>

.png)