Back
Case Series/Study
(CS-014) A Unique Technique for Management of Challenging Surgical Wounds: Treatment of a Thoracic Wound Complication with a Transforming Powder Dressing (TPD)
Co-Author(s):
Tammy Jensen Lichtman, RN, BSN, CWON – Advent Health Orlando
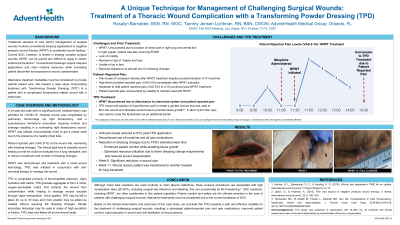
<b>Introduction</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; color: black;">Traditional standard of care (SOC) management of surgical wounds involves conventional dressing applications or negative pressure wound therapy (NPWT) to accelerate wound healing.<sup>1</sup> </span><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">Current SOC, however, is limited in treating complex surgical wounds. NPWT can be painful and difficult to apply in certain anatomical locations.<sup>2</sup> Conventional dressings require frequent applications and drain medical resources while increasing patient discomfort and exposure to wound contamination.<span style="mso-spacerun: yes;"> </span>Alternative treatment modalities must be considered to provide optimal patient care. <span style="mso-spacerun: yes;"> </span></span><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">We present a case study incorporating treatment with Transforming Powder Dressing (TPD) in a patient with a complicated thoracotomy related wound with a chest tube.</span></p><br/><br/><b>Methods</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">A 34-year-old male with no significant prior medical history was admitted for COVID-19. Hospital course was complicated by pulmonary hemorrhage s/p right thoracotomy, and a subcutaneous hematoma evacuation requiring incision and drainage resulting in a nonhealing right thoracotomy wound. NPWT was utilized unsuccessfully (hard to get a proper seal) due to the presence of a nearby chest tube. </span></p>
<p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">Patient reported constant pain (VAS 5/10) at the wound site, worse with dressing changes. The clinical goal was to expedite wound healing so that he could be evaluated for a lung transplant, and to reduce overall pain and dressing changes. </span></p><br/><br/><b>Results</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">NPWT was discontinued and TPD was initiated in conjunction with anti-microbial therapy to manage the wound. </span><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">After application of TPD, the patient experienced immediate reduction in pain. Two weeks after TPD treatment was initiated, VAS pain levels were 0/10. Dressing change requirements were substantially reduced due to TPD’s extended wear time. Overall caregiver resource utilization due to the reduction in dressing change requirements was also achieved. At week 6, a significant reduction in wound size was observed. By week 11 post start of TPD, the wound was closed, and the patient was able to be evaluated for lung transplant.</span></p><br/><br/><b>Discussion</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">Although chest tube insertions are used routinely to drain pleural collections, these invasive procedures are associated with high complication rates (20-40%), including surgical site infections and bleeding, that can occasionally be life threatening.<sup>3 </sup><span style="mso-spacerun: yes;"> </span></span><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">Patient comfort and safety are the ultimate priorities in the care of patients with challenging surgical wounds. Alternative treatments must be considered due to the current limitations of SOC. </span></p>
<p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';"> </span><span lang="EN-GB" style="font-size: 12.0pt; line-height: 110%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; mso-ansi-language: EN-GB;">Based on the clinical observations and outcomes of this case study, we conclude that TPD presents a safe and effective modality for the treatment of challenging surgical wounds.</span></p><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: 1. Harries, R. L., Bosanquet, D. C., & Harding, K. G. (2016). Wound bed preparation: TIME for an update. International wound journal, 13 Suppl 3(Suppl 3), 8–14.
2. Upton, D., & Andrews, A. (2015). Pain and trauma in negative pressure wound therapy: a review. International wound journal, 12(1), 100–105.
3. Hernandez MC, El Khatib M, Prokop L, Zielinski MD, Aho JM. Complications in tube thoracostomy: Systematic review and meta-analysis. J Trauma Acute Care Surg. 2018;85(2):410-416. doi:10.1097/TA.0000000000001840<br/><br/>
<p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">Patient reported constant pain (VAS 5/10) at the wound site, worse with dressing changes. The clinical goal was to expedite wound healing so that he could be evaluated for a lung transplant, and to reduce overall pain and dressing changes. </span></p><br/><br/><b>Results</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">NPWT was discontinued and TPD was initiated in conjunction with anti-microbial therapy to manage the wound. </span><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">After application of TPD, the patient experienced immediate reduction in pain. Two weeks after TPD treatment was initiated, VAS pain levels were 0/10. Dressing change requirements were substantially reduced due to TPD’s extended wear time. Overall caregiver resource utilization due to the reduction in dressing change requirements was also achieved. At week 6, a significant reduction in wound size was observed. By week 11 post start of TPD, the wound was closed, and the patient was able to be evaluated for lung transplant.</span></p><br/><br/><b>Discussion</b>: <p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; color: black; mso-themecolor: text1;">Although chest tube insertions are used routinely to drain pleural collections, these invasive procedures are associated with high complication rates (20-40%), including surgical site infections and bleeding, that can occasionally be life threatening.<sup>3 </sup><span style="mso-spacerun: yes;"> </span></span><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';">Patient comfort and safety are the ultimate priorities in the care of patients with challenging surgical wounds. Alternative treatments must be considered due to the current limitations of SOC. </span></p>
<p class="MsoNormal" style="text-align: justify;"><span style="font-size: 12.0pt; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman';"> </span><span lang="EN-GB" style="font-size: 12.0pt; line-height: 110%; font-family: 'Times New Roman',serif; mso-fareast-font-family: 'Times New Roman'; mso-ansi-language: EN-GB;">Based on the clinical observations and outcomes of this case study, we conclude that TPD presents a safe and effective modality for the treatment of challenging surgical wounds.</span></p><br/><br/><b>Trademarked Items</b>: <br/><br/><b>References</b>: 1. Harries, R. L., Bosanquet, D. C., & Harding, K. G. (2016). Wound bed preparation: TIME for an update. International wound journal, 13 Suppl 3(Suppl 3), 8–14.
2. Upton, D., & Andrews, A. (2015). Pain and trauma in negative pressure wound therapy: a review. International wound journal, 12(1), 100–105.
3. Hernandez MC, El Khatib M, Prokop L, Zielinski MD, Aho JM. Complications in tube thoracostomy: Systematic review and meta-analysis. J Trauma Acute Care Surg. 2018;85(2):410-416. doi:10.1097/TA.0000000000001840<br/><br/>

.png)