Back
Clinical Research
(CR-031) A real-world comparative effectiveness analysis of a bilayered living cellular construct and a dehydrated human amnion chorion membrane for use in pressure injuries
Co-Author(s):
Oscar Alvarez, PhD – Voluntary Associate Professor, Dermatology, University of Miami Miller School of Medicine
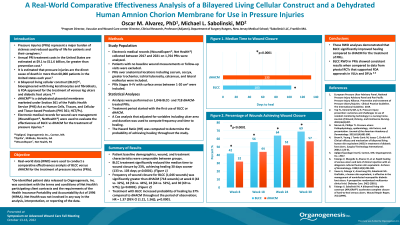
<b>Introduction</b>: <span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Using real-world data (RWD) we conducted a comparative effectiveness analysis of bilayered living cellular construct (BLCC)<sup>(<a name="_Hlk77154231"></a>a)</sup> versus <a name="_Hlk84961060"></a>a dehydrated human amnion chorion membrane (dHACM)<sup>(b)</sup> for the treatment of Pressure Injuries (PRIs). </span><br/><br/><b>Methods</b>: <p class="MsoNormal" style="margin-bottom: 0in; line-height: normal;"><span style="font-family: 'Times New Roman',serif;">Electronic medical records (WoundExpert<sup>®</sup>, Net Health, PA)<sup>(c)</sup> collected between 2017 and 2021 on 1,764 PRIs were analyzed. Ulcers 1-20 cm<sup>2</sup> were included. Patients with no baseline wound measurements or follow-up visits were excluded. Evaluations were performed on 1,046 BLCC- and 718 dHACM- treated PRIs. A Cox analysis that adjusted for variables including ulcer area and duration was used to compute frequency and time to healing. The Hazard Ratio (HR) was computed to determine the probability of achieving healing throughout the study. </span></p><br/><br/><b>Results</b>: <span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">Patient populations were well matched for patient demographics, wound characteristics, and treatment characteristics. </span><span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">The median time to healing was 133 days for dHACM and 103 days for BLCC. This difference between groups demonstrated a 23% reduction in time to healing with the use of BLCC; (p< 0.0001). T</span><span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">he frequency of healing for BLCC was significantly greater compared to dHACM at week 8 (42 vs 32%), 18 (56 vs 44%), 24 (64 vs 52%), and 30 (69 vs 57%); p< 0.0001. The HR = 1.37 [95% CI (1.21, 1.56)]; p< 0.0001. </span><br/><br/><b>Discussion</b>: <span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">These RWD analyses demonstrated that BLCC significantly improved healing compared to dHACM for the treatment of PRIs. These data may help guide clinicians’ PRI treatment practices. BLCC RWD in PRIs showed consistent results when compared to data from pivotal RCTs that supported FDA approvals in VLUs and DFUs </span><span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;"><span style="mso-no-proof: yes;">[1–3]</span></span><span style="font-size: 11.0pt; line-height: 107%; font-family: 'Times New Roman',serif; mso-fareast-font-family: Calibri; mso-fareast-theme-font: minor-latin; mso-ansi-language: EN-US; mso-fareast-language: EN-US; mso-bidi-language: AR-SA;">.</span><br/><br/><b>Trademarked Items</b>: (a) Apligraf®, Organogenesis Inc., Canton, MA
(b) EpiFix®, MiMedx, Marietta, GA
(c) WoundExpert®, Net Health, PA. De-identified patient data was consistent with the requirements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Net Health was not involved in any way in the analysis, interpretation, or reporting of the data.<br/><br/><b>References</b>: 1. Falanga V, Margolis D, Alvarez O, et al. Rapid healing of venous ulcers and lack of clinical rejection with an allogeneic cultured human skin equivalent. Arch. Dermatol. 134(3) (1998).
2. Veves A, Falanga V, Armstrong DG, Sabolinski ML. Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: A prospective randomized multicenter clinical trial. Diabetes Care. 24(2) (2001).
3. Falanga V, Sabolinski M. A bilayered living skin construct (APLIGRAF®) accelerates complete closure of hard-to-heal venous ulcers. Wound Repair Regen. 7(4) (1999).<br/><br/>
(b) EpiFix®, MiMedx, Marietta, GA
(c) WoundExpert®, Net Health, PA. De-identified patient data was consistent with the requirements of the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Net Health was not involved in any way in the analysis, interpretation, or reporting of the data.<br/><br/><b>References</b>: 1. Falanga V, Margolis D, Alvarez O, et al. Rapid healing of venous ulcers and lack of clinical rejection with an allogeneic cultured human skin equivalent. Arch. Dermatol. 134(3) (1998).
2. Veves A, Falanga V, Armstrong DG, Sabolinski ML. Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: A prospective randomized multicenter clinical trial. Diabetes Care. 24(2) (2001).
3. Falanga V, Sabolinski M. A bilayered living skin construct (APLIGRAF®) accelerates complete closure of hard-to-heal venous ulcers. Wound Repair Regen. 7(4) (1999).<br/><br/>

.png)